The risk of skin cancer in patients treated with narrowband (NB) UV-B phototherapy is not well understood. Although experimental studies have shown that there is a risk, clinical studies have not detected an increased incidence of cancer following treatment. The aim of this study was to determine the incidence of nonmelanoma skin cancer (NMSC) in patients treated with NB UV-B phototherapy at a tertiary care hospital in the Mediterranean area.
Material and methodsWe conducted a retrospective chart review of 474 patients who received whole-body NB UV-B phototherapy at our hospital between 2002 and 2016 and identified those diagnosed with NMSC during follow-up. We calculated the corresponding crude and standardized incidence rates and compared these with rates in the general population in a similar geographic area.
ResultsOf the 474 patients, 193 (40.7%) were men and 281 (59.3%) were women. The mean (SD) follow-up period was 5.8 (3) years. The prevalence of NMSC at the end of the study period was 1.9% and the standardized incidence was 108.3 cases per 100 000 patient-years. The SIR of 1.9 in the study group was not significantly different from that of the general population. The number of patients who needed to be treated with NB UV-B phototherapy for 1 case of NMSC to occur was 1900.
ConclusionNB UV-B phototherapy does not appear to be associated with an increased risk of NMSC
Actualmente el riesgo de cáncer cutáneo asociado a la fototerapia UVB de banda estrecha no se conoce con precisión. Aunque existe un riesgo demostrado en estudios experimentales los estudios en la práctica clínica no han encontrado un aumento en la frecuencia de neoplasias en los pacientes tratados con esta modalidad de fototerapia. El objetivo de nuestro trabajo es determinar la incidencia de fotocarcinogénesis de la fototerapia UVB-BE en un hospital terciario del área mediterránea.
Material y métodoSe ha realizado un estudio observacional retrospectivo selecionando 474 pacientes que habían recibido tratamiento con UVB-BE de cuerpo completo entre 2002 y 2016 realizando un seguimiento en la historia clínica revisando los pacientes que habían sido diagnosticados de CCNM. Se calculó la densidad de incidencia bruta y ajustada y se comparó con la frecuencia en la población normal de un area geográfica similar.
ResultadosDe los 474 pacientes estudiados, 193 eran hombres (40,7%) y 281 mujeres (59,3%). El tiempo medio de seguimiento fue de 5,8+-3 años. La prevalencia de neoplasias al final del periodo de estudio fue del 1,9% La densidad de incidencia ajustada fue de 108,3 casos / 100.000 pacientes tratados – año. La relación estandarizada de riesgo en comparación con la población general fue de 1,9 sin llegar a ser estadísticamente significativa. El número necesario a tratar para producir un caso de cáncer cutáneo fue de 1.900 pacientes.
ConclusiónLa fototerapia UVB-BE no parece asociarse con un riesgo aumentado de cáncer cutáneo no melanoma en los pacientes tratados con esta modalidad de tratamiento.
Phototherapy is a physical treatment modality based on ultraviolet light that is widely used in dermatology. The most widely used modality today is narrowband (NB) UV-B phototherapy, owing to its safety and convenience.1
Despite being a relatively safe technique, NB UV-B phototherapy causes concern, mainly because of the hypothetical risk of nonmelanoma skin cancer (NMSC).
The photocarcinogenic risk of other phototherapy modalities, such as psoralen UV-A (PUVA), is well recognized.2,3 This risk has proven greater for cutaneous squamous cell carcinoma (SCC), especially on the lower limbs.4
Experimental studies have shown the carcinogenic effects of broadband UV-B phototherapy. NB UV-B has proven to be more carcinogenic than broadband UV-B in animals.5,6 Nevertheless, no clinical practice–based study has managed to demonstrate an increased risk of NMSC or melanoma associated with NB UV-B phototherapy.2
The incidence of NMSC varies considerably according to several factors (eg, geographic region, skin phototype, and sun exposure habits). Therefore, caution should be exercised when extrapolating the findings of epidemiological studies on NMSC performed in specific geographical regions to other populations. In the case of the Spanish population, several studies have determined the incidence of NMSC in populations from different geographic areas.7
As for data on NMSC in patients treated with NB UV-B, current studies in the Mediterranean area are scarce and heterogeneous and based on small samples.8,9
Under the working hypothesis that NB UV-B phototherapy has a low or nonexistent risk of carcinogenesis, the main objective of the present study was to determine the incidence of skin cancer in patients treated with NB UV-B phototherapy and to compare it with the incidence among the general population in a similar geographic area.
Material and MethodsWe performed a retrospective observational study of 474 patients who had received full-body NB UV-B phototherapy between 2002 and 2016 at the Photobiology and Phototherapy Unit of Hospital General Universitario de Valencia (HGUV), Valencia, Spain.
The inclusion and exclusion criteria are set out below.
Inclusion criteria
- •
Skin disease treated with NB UV-B phototherapy at the Photobiology and Phototherapy Unit of HGUV between 2002 and 2016.
- •
Data from at least 1 year of follow-up.
Exclusion criteria
- •
Treatment with a phototherapy modality other than NB UV-B before treatment with NB UV-B or before the appearance of the first tumor.
Patients received NB UV-B phototherapy using the Waldmann UV-7002 or Waldmann UV-7001K system. The treatment protocols were those recommended by the Spanish Photobiology Group (Grupo Español de Fotobiología).10
Clinical and treatment-related data were retrieved from the records of the Photobiology and Phototherapy Unit of HGUV. A retrospective follow-up was performed to investigate the appearance of skin cancer over time. Patients were followed up by accessing data from the Unified Electronic Clinical History of the Autonomous Community of Valencia (ABUCASIS) and the database of the dermatopathology laboratory of HGUV. The only cases considered positive were those in which the suspicious lesion was confirmed by histopathology. Following the recommendations of epidemiological studies on skin cancer, only the first tumor for each histologic type and patient was considered a case of NMSC.7 For each case, the date the tumor appeared was recorded, as were the location and the definitive histological diagnosis.
The date of the last face-to-face visit at the Dermatology Department of our hospital was recorded for all patients in order to establish the individual follow-up period. The incidence density of NMSC was calculated, as was the age-adjusted incidence density following the direct standardization method for age and sex in the world population described by Segi et al.11
ResultsCharacteristics of the Study PopulationWe analyzed data from 474 patients treated with NB UV-B phototherapy between 2002 and 2016 and who had been followed for at least 1 year. There were 193 men (40.7%) and 281 women (59.3%). The patients’ characteristics are shown in Table 1.
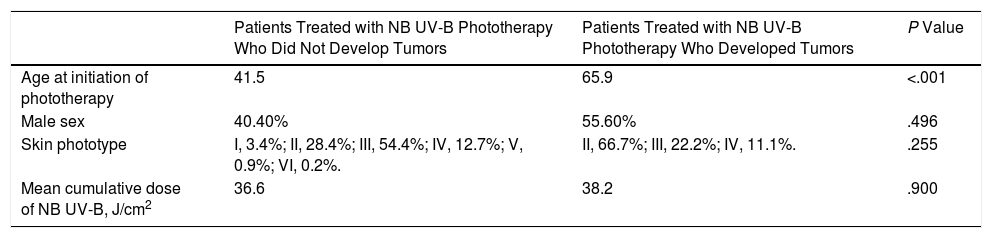
Epidemiological Characteristics of Patients Treated with NB UV-B Who Developed and Did Not Develop NMSC.
| Patients Treated with NB UV-B Phototherapy Who Did Not Develop Tumors | Patients Treated with NB UV-B Phototherapy Who Developed Tumors | P Value | |
|---|---|---|---|
| Age at initiation of phototherapy | 41.5 | 65.9 | <.001 |
| Male sex | 40.40% | 55.60% | .496 |
| Skin phototype | I, 3.4%; II, 28.4%; III, 54.4%; IV, 12.7%; V, 0.9%; VI, 0.2%. | II, 66.7%; III, 22.2%; IV, 11.1%. | .255 |
| Mean cumulative dose of NB UV-B, J/cm2 | 36.6 | 38.2 | .900 |
Abbreviations: NB, narrowband; NMSC, nonmelanoma skin cancer.
Mean (SD) follow-up time was 5.8 (3) years (range, 1.1-14.5). Cumulative follow-up time was 2750 patient-years. Mean age at the end of follow-up was 47.5 (20.6) years (range, 6.7-98).
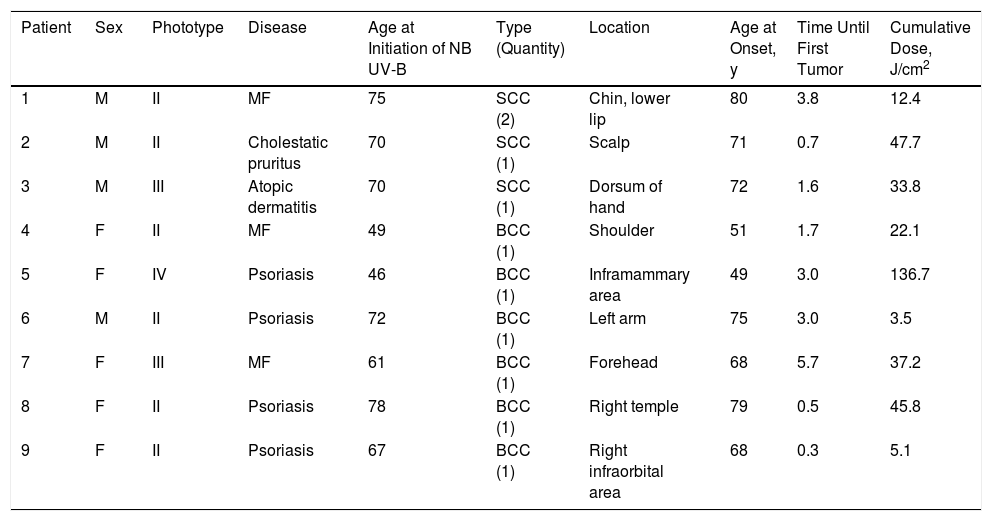
Tumors DetectedTen tumors were diagnosed in 9 patients during follow-up, that is, a prevalence of 1.9% at the end of the study period. The tumors were basal cell carcinoma (BCC) in 6 cases and SCC in 4 cases. Taking into account a single case per histologic type, the prevalence of BCC was 1.3% and that of SCC was 0.6%.
When all the lesions diagnosed were taken into account, the prevalence of NMSC was 2.1%. The prevalence of BCC was 1.3% and that of SCC was 0.6%.
Mean age at initiation of phototherapy was higher in patients with tumors (Table 1). No statistically significant differences were found for sex, skin phototype, or cumulative dose of NB UV-B, regardless of whether or not the patient had developed a tumor.
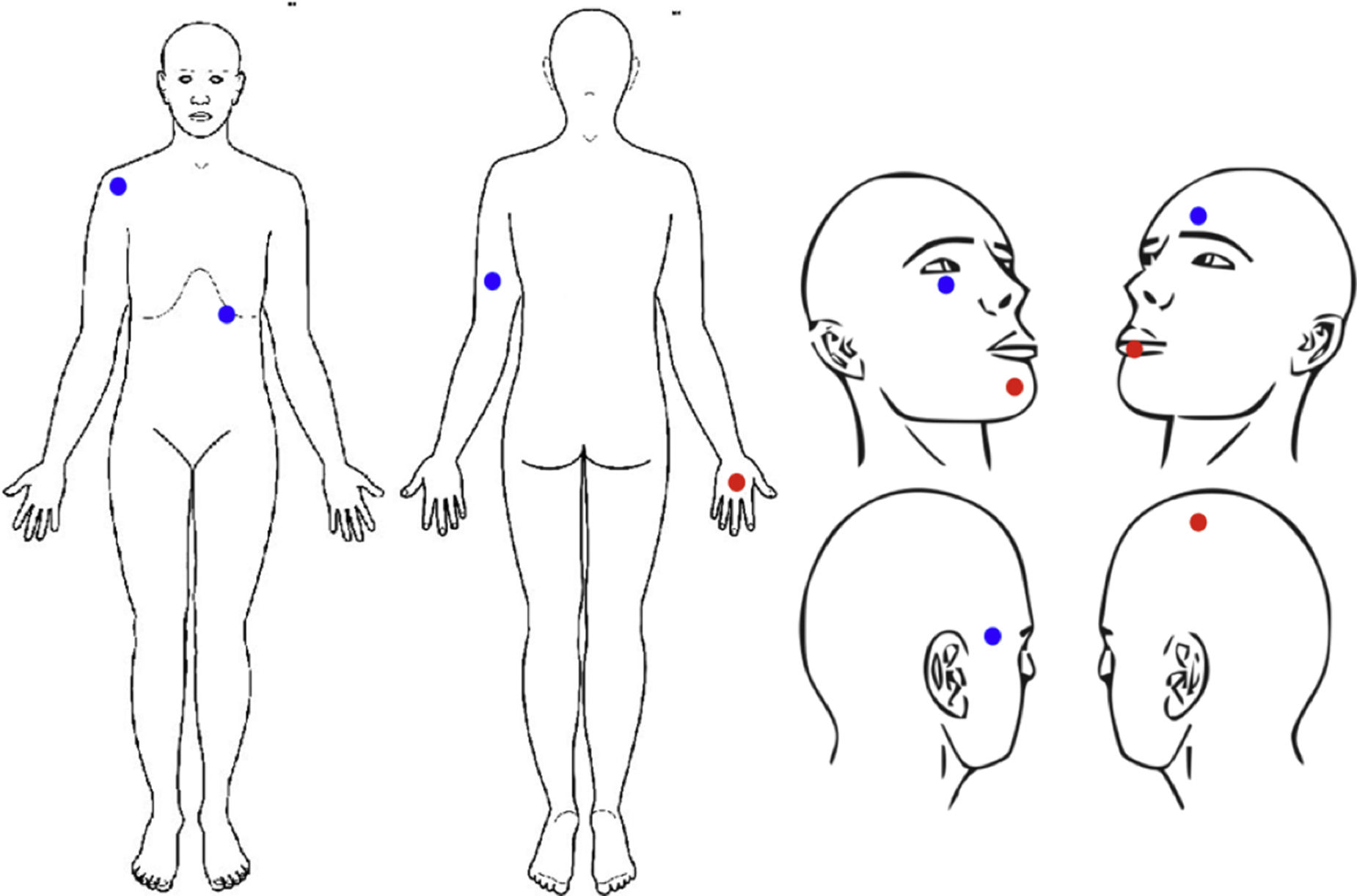
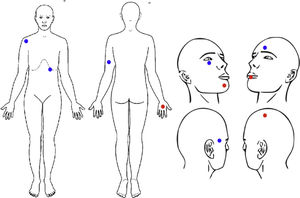
The location of the lesions is shown in Figure 1. Lesions were on the head in 6 cases (60%, 3 SCC and 3 BCC), the upper limbs in 3 cases (30%, 2 BCC and 1 SCC), and the trunk in 1 case (10%, 1 BCC) (Table 2).
Characteristics of Patients Who Developed Tumors.
| Patient | Sex | Phototype | Disease | Age at Initiation of NB UV-B | Type (Quantity) | Location | Age at Onset, y | Time Until First Tumor | Cumulative Dose, J/cm2 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | II | MF | 75 | SCC (2) | Chin, lower lip | 80 | 3.8 | 12.4 |
| 2 | M | II | Cholestatic pruritus | 70 | SCC (1) | Scalp | 71 | 0.7 | 47.7 |
| 3 | M | III | Atopic dermatitis | 70 | SCC (1) | Dorsum of hand | 72 | 1.6 | 33.8 |
| 4 | F | II | MF | 49 | BCC (1) | Shoulder | 51 | 1.7 | 22.1 |
| 5 | F | IV | Psoriasis | 46 | BCC (1) | Inframammary area | 49 | 3.0 | 136.7 |
| 6 | M | II | Psoriasis | 72 | BCC (1) | Left arm | 75 | 3.0 | 3.5 |
| 7 | F | III | MF | 61 | BCC (1) | Forehead | 68 | 5.7 | 37.2 |
| 8 | F | II | Psoriasis | 78 | BCC (1) | Right temple | 79 | 0.5 | 45.8 |
| 9 | F | II | Psoriasis | 67 | BCC (1) | Right infraorbital area | 68 | 0.3 | 5.1 |
Abbreviations: BCC, basal cell cancer; MF, mycosis fungoides; NB, narrowband; NMSC, nonmelanoma skin cancer; SCC, squamous cell cancer.
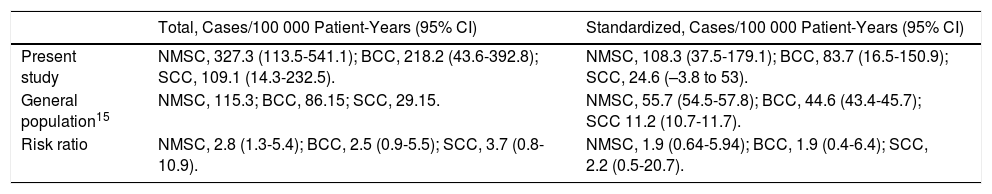
Based on a single case per tumor and histologic type, the incidence density of NMSC in patients treated with NB UV-B phototherapy was 327.3/100 000 patient-years (95% CI, 113.5-541.1). After direct standardization adjusted for the age of the world population, the adjusted incidence density of NMSC was 108.3 cases per 100 000 patient-years (95% CI, 37.5-179.1).
DiscussionOur results confirm the initial hypothesis that the carcinogenic risk of NB UV-B phototherapy is low or nonexistent.
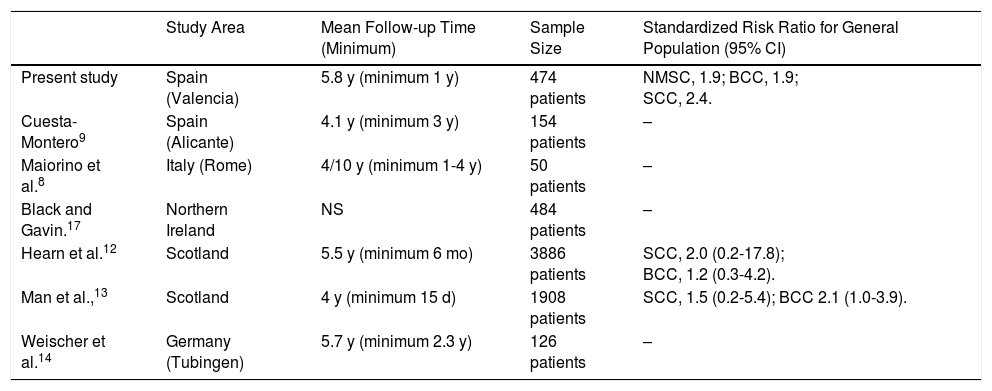
Our study is the largest to date on photocarcinogenesis in the Mediterranean area. The mean follow-up time of 5.8 years is similar to that of all previous studies on NB UV-B phototherapy (Table 3). The sample is the largest to date in the Mediterranean area,8,9 although much lower than that of the 2 main studies on photocarcinogenesis associated with NB UV-B phototherapy.12,13
Total and Standardized Incidence Density of Skin Tumors in Patients Treated With NB UV-B Phototherapy in Our Study and in the Healthy Population in Girona. Risk of NMSC in Patients Treated With NB UV-B Phototherapy in Our Study.
| Total, Cases/100 000 Patient-Years (95% CI) | Standardized, Cases/100 000 Patient-Years (95% CI) | |
|---|---|---|
| Present study | NMSC, 327.3 (113.5-541.1); BCC, 218.2 (43.6-392.8); SCC, 109.1 (14.3-232.5). | NMSC, 108.3 (37.5-179.1); BCC, 83.7 (16.5-150.9); SCC, 24.6 (–3.8 to 53). |
| General population15 | NMSC, 115.3; BCC, 86.15; SCC, 29.15. | NMSC, 55.7 (54.5-57.8); BCC, 44.6 (43.4-45.7); SCC 11.2 (10.7-11.7). |
| Risk ratio | NMSC, 2.8 (1.3-5.4); BCC, 2.5 (0.9-5.5); SCC, 3.7 (0.8-10.9). | NMSC, 1.9 (0.64-5.94); BCC, 1.9 (0.4-6.4); SCC, 2.2 (0.5-20.7). |
Abbreviations: BCC, basal cell cancer; NB, narrowband; NMSC, nonmelanoma skin cancer; SCC, squamous cell cancer.
Mean age at the end of follow-up (47.5 [20.6] years) was similar to that found elsewhere. Weischer et al.14 reported age at the end of follow-up to be 51.2 years; Hearn et al.12 reported it to be 39.5 years.
Minimum follow-up time is very short in some studies,12,13 and no other studies report the cumulative time period in patient-years except Hearn et al.12 (24 753 patient-years). The number of patient-years is a more reliable indicator of the total observation period than total follow-up time. As this is an arithmetic measure, the mean follow-up time loses validity when used in bimodal distributions.
We detected skin tumors in 1.9% of patients at the end of the study period. This figure is lower that that reported by Maiorino et al.8 (12%) and by Cuesta-Montero9 (5.2%) but similar to that of other larger-scale studies such as that of Hearn et al.12 (1%) and Man et al.13 (0.7%). The high prevalence reported in some studies8,9 may be overestimated because of the low sample size.
The most frequent histological form detected was BCC (60%). This finding is consistent with those of other studies9,12–14 and similar to the percentage of this histologic type with respect to the total for NMSC in the general population (74.7%).15
The greater frequency of BCC contrasts with the findings reported for patients treated with PUVA in other studies, which showed SCC to be the most common tumor.2 The high percentage of SCC is one of the factors thought to be associated with the carcinogenic effect of phototherapy; consequently, the lower frequency of this tumor in the present study supports the lesser carcinogenic effect of this modality.
The total cumulative dose was similar in patients who developed skin tumors and in those who did not, with no significant differences. This finding could indicate that NB UV-B radiation has no clear dose-dependent carcinogenic effect or that it did not reach the carcinogenic threshold for this treatment modality. The differences detected in our study are clinically irrelevant (38.2J/cm2 vs 36.6J/cm2); therefore, it is unlikely that studies with a larger sample size would yield clinically significant results.
Age at initiation of phototherapy was higher in patients with tumors, possibly because, as the follow-up period was relatively short, patients who started phototherapy at an older age were followed for longer, thus increasing the cumulative risk of NMSC. This potential bias was corrected using the standardized incidence rate.
The most frequent location of the skin lesions was the head and upper limbs, consistent with findings for the general population.16 No patients developed skin tumors on the legs, in contrast with patients treated with PUVA, in whom the lower limbs are one of the most frequently affected sites.4 The absence of lesions at this site is yet another indicator suggesting that the carcinogenic effect of NB UV-B radiation is lower than that of PUVA phototherapy.
The incidence density of skin tumors was 327.3/100 000 patient-years, which is much higher than in the general population (115.3/100 000 patient-years).15 However, this result is difficult to compare, because it depends to a large extent on the age of the study population, which in the present case comprises adults followed over a more or less prolonged time period.
In contrast with the prevalence of NMSC, no study to date has reported the incidence density of NMSC or of its clinical forms in patients treated with NB UV-B phototherapy.8,9,12–14,17
Standardization for age and sex revealed an incidence density of NMSC lower than the gross density (108.3 vs 327.3), thus confirming that the sample studied was from an aging population (as a result of the length of the follow-up period). Therefore, the carcinogenic effect of NB UV-B phototherapy would be overestimated without standardization for age.
Comparison of the incidence density of skin tumors with that of the population of Girona described by Vilar-Coromina15 (Table 3) revealed a standardized risk ratio of 1.9, which was not statistically significant.
The standardized risk ratio compared with the healthy population was obtained in the studies by Hearn et al.12 and Man et al.13 (Table 4). In neither case was a potential carcinogenic effect of NB UV-B phototherapy demonstrated. However, it is noteworthy that all of the studies performed show a standardized risk ratio that leans positively toward NB UV-B phototherapy, indicating potentially significant differences that could not be appreciated because of the low sample size. Studies with longer follow-up periods would be advisable if we wish to increase the number of cases detected and the statistical power of the comparative tests.
Characteristics and Results of All Studies on the Photocarcinogenic Risk of NB UV-B Phototherapy Published in the Literature.
| Study Area | Mean Follow-up Time (Minimum) | Sample Size | Standardized Risk Ratio for General Population (95% CI) | |
|---|---|---|---|---|
| Present study | Spain (Valencia) | 5.8 y (minimum 1 y) | 474 patients | NMSC, 1.9; BCC, 1.9; SCC, 2.4. |
| Cuesta-Montero9 | Spain (Alicante) | 4.1 y (minimum 3 y) | 154 patients | – |
| Maiorino et al.8 | Italy (Rome) | 4/10 y (minimum 1-4 y) | 50 patients | – |
| Black and Gavin.17 | Northern Ireland | NS | 484 patients | – |
| Hearn et al.12 | Scotland | 5.5 y (minimum 6 mo) | 3886 patients | SCC, 2.0 (0.2-17.8); BCC, 1.2 (0.3-4.2). |
| Man et al.,13 | Scotland | 4 y (minimum 15 d) | 1908 patients | SCC, 1.5 (0.2-5.4); BCC 2.1 (1.0-3.9). |
| Weischer et al.14 | Germany (Tubingen) | 5.7 y (minimum 2.3 y) | 126 patients | – |
Abbreviations: BCC, basal cell cancer; NB, narrowband; NMSC, nonmelanoma skin cancer; NS, not specified; SCC, squamous cell cancer.
The median age at diagnosis of the skin tumors in patients treated with NB UV-B phototherapy was 71.5 years. This finding contrasts with the mean age of the population at the end of the study (47.5 years), thus highlighting the importance of performing studies with long follow-up periods and especially studies that assess patients to an older age. The carcinogenic risk of NB UV-B phototherapy seems to be a late phenomenon that does not appear immediately after treatment but rather is added to the patient's baseline risk, with onset of the skin tumors at the usual age of presentation (sixth and seventh decades of life).
The adjusted risk of NMSC attributable to exposure to NB UV-B compared with the general population15 is 52.6 cases per 100 000 patient-years, that is, 1900 patients would need to be treated with the habitual doses of NB UV-B for 1 case of treatment-associated NMSC to occur. This number needed to harm is very low given the habitual volume of patients treated at a phototherapy unit. Therefore, our results show that the risk of NMSC caused by NB UV-B phototherapy is very low and that this modality can be used safely in daily clinical practice.
In conclusion, consistent with other studies, we were unable to demonstrate a clinically relevant carcinogenic effect associated with NB UV-B phototherapy. Nevertheless, we cannot conclude that this treatment modality is risk-free. Therefore, studies with longer follow-up periods are essential if we are to confirm or rule out the carcinogenic risk of NB UV-B phototherapy.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ortiz-Salvador JM, Ferrer DS, Saneleuterio-Temporal M, Victoria Martínez AM, Ferriols AP, Vilata Corell JJ, et al. Riesgo de fotocarcinogénesis asociado a la fototerapia UVB-BE. Estudio epidemiológico de un hospital terciario. Actas Dermosifiliogr. 2018;109:340–345.