This study was aimed to examine patients’ knowledge, behaviours and attitudes regarding actinic keratosis (AK) lesions and the impact of the disease on patients’ quality of life (QoL).
MethodsObservational study of patients with AK lesions in Spain. QoL was evaluated with the validated version of Spanish AKQoL questionnaire. Skin self-examination, sun-exposure, habits and attitudes towards AK's treatment were recorded using different questionnaires. The adherence was assessed by means of the Morisky-Green test. Among other variables, QoL and adherence to treatment were compared by using Pearson's χ2 test and one-way ANOVA tests. Inferential analysis regarding such factors and length of treatment were also performed.
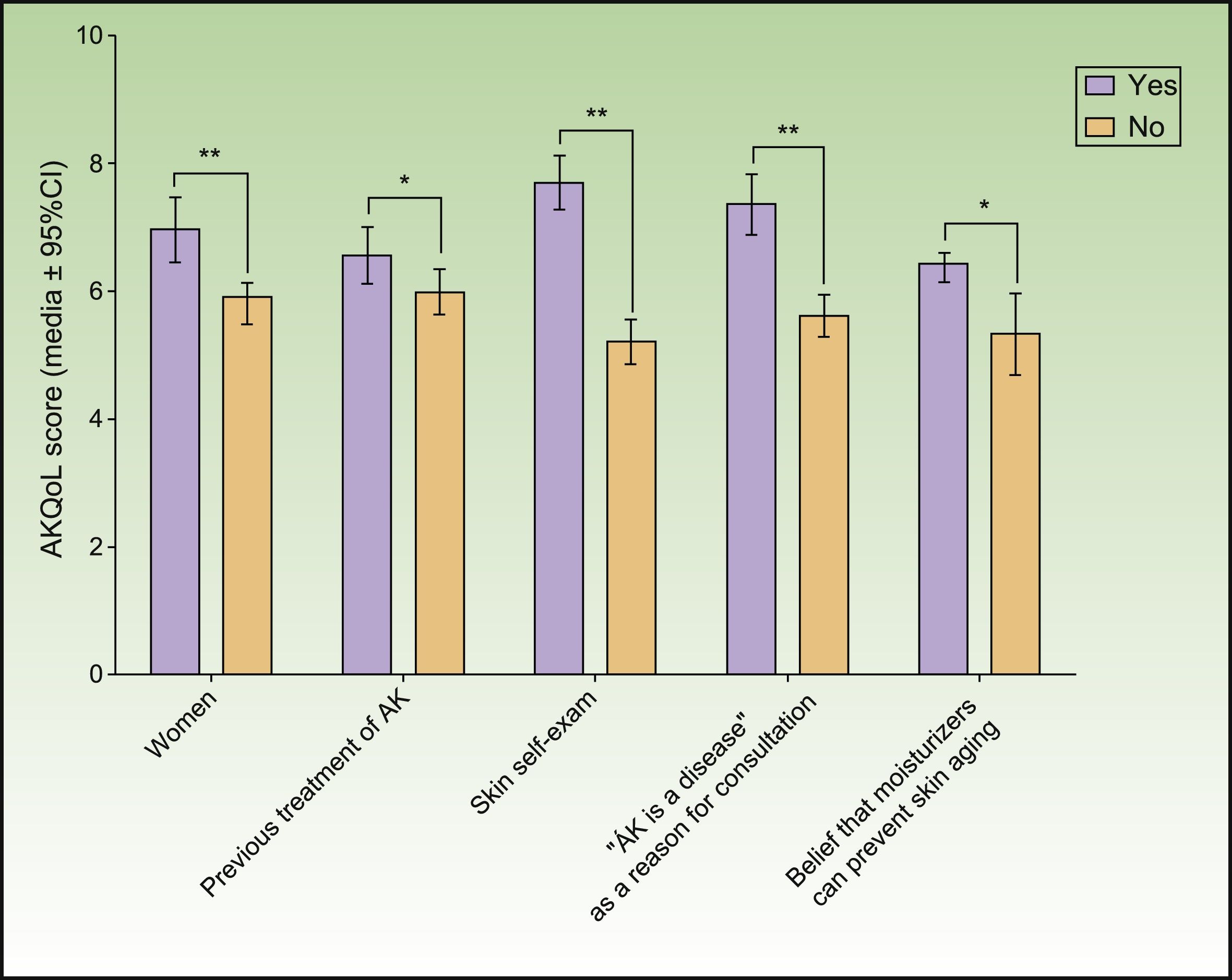
ResultsA total of 1240 patients (73.6 [10.5] years old) were recruited. Overall, patients that showed higher levels of concern were also showed a higher impairment on QoL. AK had greater effects on women's QoL and those who performed skin self-examination, think that AK is a disease and/or believe that moisturizers can prevent skin aging (P<.05). Adherence and length of treatment were strongly related, since patients with treatments intended for <1week were more likely to show good adherence and complete remission of AK (Odds Ratio [95%CI]: 6.25 [4.55-8.33] and 2.63 [1.96-3.45]), respectively).
ConclusionsConcerns due to AK are mainly related to sex and to the consideration of AK as a disease. More concerned patients tend to have lower QoL and good adherence to treatment. Short length of treatment was associated with better adherence and complete remission of AK lesions.
El objetivo de este estudio fue examinar el conocimiento, el comportamiento y las actitudes de los pacientes hacia las lesiones de queratosis actínica (QA) y cómo esta enfermedad influye en la calidad de vida (CV).
MétodosEstudio observacional de pacientes con lesiones de QA en España. La CV se evaluó con la versión española del Cuestionario de Calidad de Vida en pacientes con Queratosis Actínica (AKCV). El autoexamen de la piel, la exposición al sol y los hábitos y actitudes hacia el tratamiento de la QA quedaron registrados a través de diferentes cuestionarios. La adherencia al tratamiento fue valorada utilizando el test de Morisky-Green. Entre otras variables, la CV y la adherencia al tratamiento se compararon mediante la prueba de χ2 de Pearson y las pruebas ANOVA de un factor. También se llevó a cabo un análisis inferencial tanto de estas variables como de la duración del tratamiento.
ResultadosSe reclutaron un total de 1.240 pacientes (73,6 [10,5] años). En líneas generales, los pacientes que mostraron mayores niveles de preocupación también mostraron un mayor deterioro de la CV. La QA tuvo mayores efectos sobre la CV de las mujeres, sobre los pacientes que realizaban autoexploraciones de la piel, y sobre los que piensan que la QA es una enfermedad y/o creen que los hidratantes son capaces de prevenir el envejecimiento de la piel (p<0,05). Tanto la adherencia como la duración del tratamiento guardaron una estrecha relación, ya que los pacientes con tratamientos de menos de una semana de duración tenían más probabilidades de mostrar una buena adherencia y una remisión completa de la QA (cociente de odds u odds ratio: OR [IC95%]: 6,25 [4,55-8,33] y 2,63 [1,96-3,45], respectivamente).
ConclusionesLas preocupaciones que hay en torno a la QA se asocian, principalmente, al sexo y a que la QA se considera una enfermedad. Los más preocupados suelen tener una CV más baja y una buena adherencia al tratamiento. Una duración corta del tratamiento se asoció a una mejor adherencia y a una remisión completa de las lesiones de QA.
The presence of Actinic Keratosis (AK) lesions on photo-exposed areas like the face and scalp is relatively common in Spanish population and is one of the main reasons for consultation to dermatologist.1–4,25 The clinical significance of AK relates to the risk of malignant transformation to nonmelanoma skin cancer (NMSC), including squamous cell carcinoma (SCC).
Because it is impossible to predict whether a given AK will regress, persist, or progress, AKs should be ideally treated,5 especially in immunosuppressed individuals and those with a history of NMSC.6,7 Most treatments (lesion-directed and field-directed) significantly reduce AK lesions, but may elicit a range of local skin responses which usually have a negative impact on Quality of Life (QoL).8 Furthermore, some treatments have a long duration that may negatively affect adherence to treatment9 that is associated with poor response to treatment and worse disease outcome.10,11 Consequently, current guidelines and expert consensus advocate choosing a treatment schedule based not only on AK-related factors but taking into account patients’ characteristics, expectations, opinions and preferences as well.4,12,25
General practice establishes that primary prevention of sun-related skin diseases requires the adoption of educational measures regarding sun-protective behaviours13 and other actions in order to raise people's awareness about the real danger of these diseases.14 Non-consideration of AK as a threat constitutes a barrier for many people in the acquisition of healthy sun exposure habits.15 Indeed, this kind of misconceptions should be seriously considered since these may influence negatively some relevant factors, not only in AK prevention, but also adherence to its treatment.16
In this scenario, the aim of this study was to examine patients’ knowledge, behaviours and attitudes regarding AK lesions, and also to assess the impact of this disease on their QoL.
MATERIALS AND METHODSSetting and populationA multicentre, prospective and observational study was conducted by 191 dermatologists from all over Spain to obtain a representative sample of the territory. The study was conducted in accordance with the Declaration of Helsinki (Fortaleza, 2013) and the Good Clinical Practices. All the study's materials were reviewed and approved by ethical committee of Hospital General Universitario Gregorio Marañón (Madrid), and all patients were asked to provide written consent before inclusion. The sample comprised consecutive patients over 18 years old who consulted their dermatologist between January and November 2014 and presented AK lesions at time of inclusion.
Demographics and dermatological profile data were collected at baseline: demographics (age, sex, level of education), reason for consultation (aesthetic concern, believe that AK is a disease, doctor's indication, relatives or friends’ advice); dermatological profile (Fitzpatrick phototype,17 previous treatments for AK (yes/no), number, location and clinical classification of AK lesions that require treatment, length of treatment indicated by the dermatologist (1 day, <1 week, > 2 weeks, >4 weeks). It was not contemplated to perform biopsies of the lesions for this study.
To evaluate habits, attitudes, and understanding of exposure to sunlight, four subscales of the “beach questionnaire”15 were used:
- 1.
Habits of sun exposure on the beach (3 items with Likert format) as a mean of days and number of hours.
- 2.
Sunburns on the beach (1 item with Likert format): sunburn is defined as the presence of redness and pain after sun exposure.
- 3.
Sun protection practices on the beach (6 items with Likert format): put in the shade, wear sunglasses, wear a hat or cap, wear Long-sleeved clothing or long pants, avoid sun during the middle of the day and use high sunscreen.
- 4.
Knowledge about sun exposure (7 items with dichotomous responses).
An additional item was added to evaluate if patients used to expose themselves to the sun at the moment of the baseline visit (dichotomous response), regardless it was during walks, at the beach, parks or in other circumstances.
To evaluate patients’ concern about AK, dermatologists asked patients about the frequency of skin self-examination and medical dermatologic visits and use of tanning lamps. The following pool of questions were also assessed to evaluate patients’ perceptions about AK with dichotomous format of responses: awareness of AK as a disease, need of treatment, need to avoid sun-exposure. Finally, the dermatologist evaluated the patient's acceptance of the therapeutic plan (rated on a generic numeric scale ranging from 0 (none) to 10 (complete)). items.
Quality of Life (QoL) was evaluated with the Spanish version of the Actinic Keratosis Quality of Life Questionnaire (AKQoL).18 The AKQoL, originally proposed by Esmann et al,12 was adapted and validated for our group and allows assessment of the impact of AK on patients’ QoL. It is composed of three domains or subscales: emotions (fear, guilt, shame, worry and irritation/bother), function (personal views of QoL, social life and appearance) and control over life in general. The questionnaire comprises nine items scored on a 4-point scale ranging from 0 (rarely/not at all) to 3 (very much/all the time). The total possible score ranges from 0 to 27 with higher scores indicating greater impairment of QoL.
Follow-up visits were performed between one and three months after baseline in patients receiving therapy for AK in order to obtain data about adherence to treatment and clinical outcomes.
Adherence to treatment was evaluated by means of the dermatologist's estimate of the proportion of days with correct application of treatment (100% of days: complete adherence; ≥80%: correct adherence and <80%: non-adherence) and by Morisky-Green test - MGT,19 a self-reported measure of medication taking with four items that patients were asked to complete at home before the follow up visit.
Clinical outcomes (complete remission and treatment discontinuation) were also collected and recorded by dermatologists at the follow up visit.
Statistical analysisContinuous variables were summarized and are presented as the number of valid cases (n), as means (standard deviation) (SD), medians and percentiles, and extreme values (minimum and maximum), while categorical variables are described by the number of valid cases and percentage of each category. Comparisons between groups were performed using Pearson's Chi-square tests for categorical variables and one-way ANOVA tests for numerical variables. Inferential analysis was performed for variables such as length of treatment (<1 week or ≥2 weeks), adherence (according to the MGT) and impairment on QoL (mean score of AKQoL). The associations between the “beliefs and attitudes of patients” and “length of treatment” with “adherence to treatment” and the association between “clinical outcome” and “length of treatment” were presented as Odds Ratio (OR) with Confidence Intervals at 95% [95%CI]. Patients with a single-day treatment were excluded when analysing these associations.
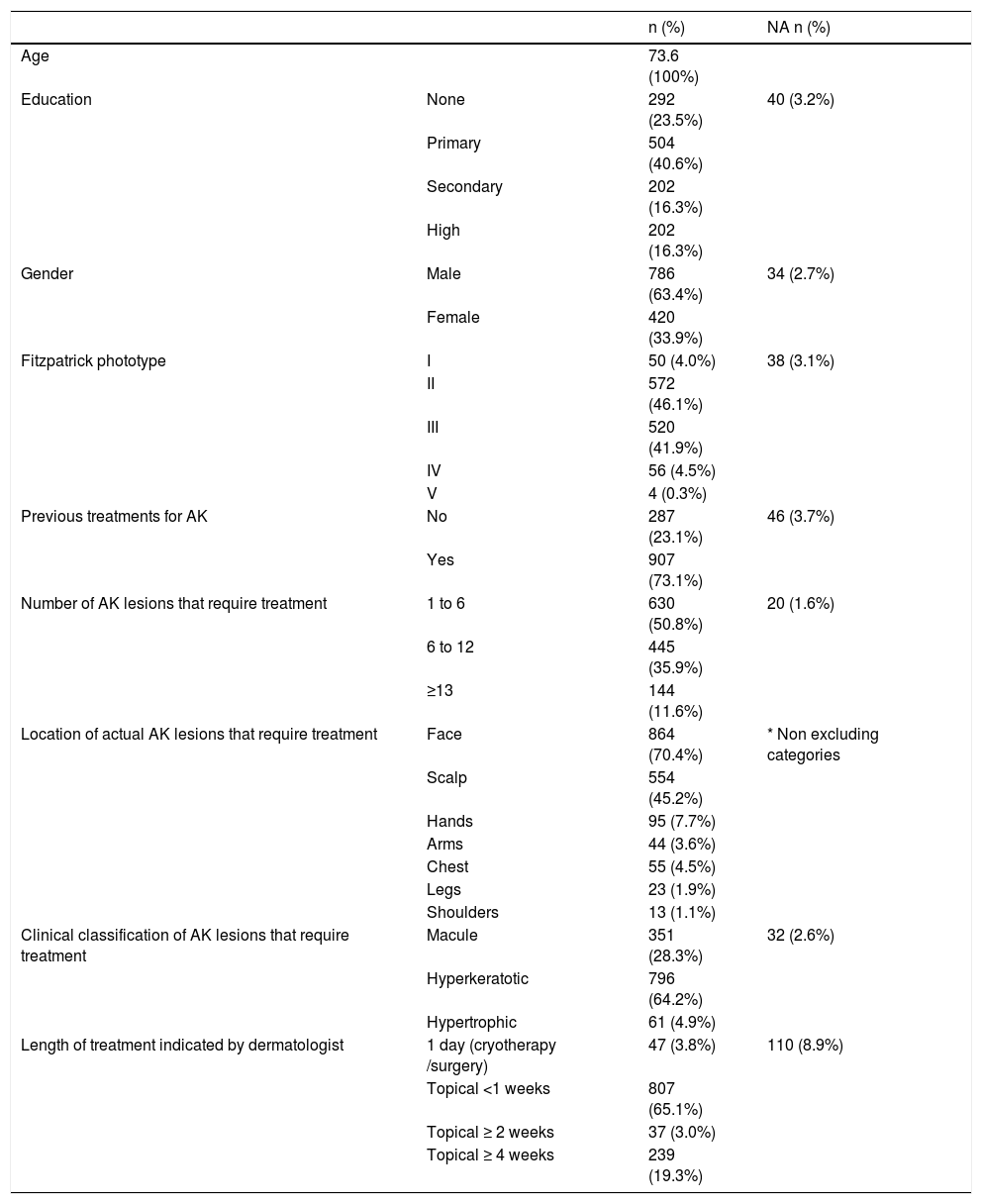
RESULTSDemographics and dermatological profileA total of 1240 patients (mean age 73.6 (10.55) years, range 31 - 98 years) were included in the study and 1159 (93.5%) of them completed it. Main reasons for consultation to dermatologist were “physician referral” (59.2%) and “think that AK is a disease” (35.2%).
AK lesions were most frequently located on the face and scalp with an average duration of 13.4 (6 months). Treatment for AK was prescribed attending to the differences between the AK lesions presented in patients. One to five clinically visible AK lesions were found in the intended-to-treat area in 50.8% of cases, 35.9% presented six to twelve clinically visible AK and 11.6% presented more than 12 lesions. There were 76% of patients with AK history prior to inclusion in the study. The 66% of patients received treatment following a previous indication; almost 37% of patients had been previously treated regarding older lesions, and a 23.2% received treatment at their own request.
For more details about patients’ characteristics and dermatological profile see Table 1.
Patients’ characteristics and dermatological profile.
| n (%) | NA n (%) | ||
|---|---|---|---|
| Age | 73.6 (100%) | ||
| Education | None | 292 (23.5%) | 40 (3.2%) |
| Primary | 504 (40.6%) | ||
| Secondary | 202 (16.3%) | ||
| High | 202 (16.3%) | ||
| Gender | Male | 786 (63.4%) | 34 (2.7%) |
| Female | 420 (33.9%) | ||
| Fitzpatrick phototype | I | 50 (4.0%) | 38 (3.1%) |
| II | 572 (46.1%) | ||
| III | 520 (41.9%) | ||
| IV | 56 (4.5%) | ||
| V | 4 (0.3%) | ||
| Previous treatments for AK | No | 287 (23.1%) | 46 (3.7%) |
| Yes | 907 (73.1%) | ||
| Number of AK lesions that require treatment | 1 to 6 | 630 (50.8%) | 20 (1.6%) |
| 6 to 12 | 445 (35.9%) | ||
| ≥13 | 144 (11.6%) | ||
| Location of actual AK lesions that require treatment | Face | 864 (70.4%) | * Non excluding categories |
| Scalp | 554 (45.2%) | ||
| Hands | 95 (7.7%) | ||
| Arms | 44 (3.6%) | ||
| Chest | 55 (4.5%) | ||
| Legs | 23 (1.9%) | ||
| Shoulders | 13 (1.1%) | ||
| Clinical classification of AK lesions that require treatment | Macule | 351 (28.3%) | 32 (2.6%) |
| Hyperkeratotic | 796 (64.2%) | ||
| Hypertrophic | 61 (4.9%) | ||
| Length of treatment indicated by dermatologist | 1 day (cryotherapy /surgery) | 47 (3.8%) | 110 (8.9%) |
| Topical <1 weeks | 807 (65.1%) | ||
| Topical ≥ 2 weeks | 37 (3.0%) | ||
| Topical ≥ 4 weeks | 239 (19.3%) |
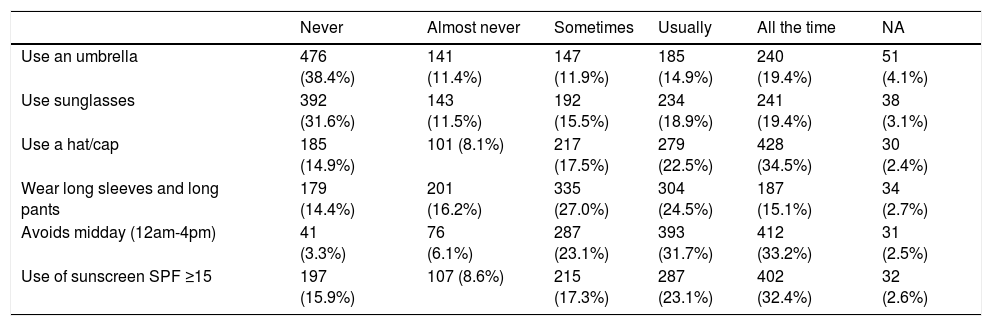
At baseline, 53.4% patients reported daily sun-exposure, mostly during daily walks. Approximately 40% had sunbathed at the beach, parks or other places eventually for more than 30 days in the last year. Use of tanning lamps was reported only in 19 cases. Photoprotective measures during sun exposure are described in Table 2.
Photoprotective measures during sun exposure.
| Never | Almost never | Sometimes | Usually | All the time | NA | |
|---|---|---|---|---|---|---|
| Use an umbrella | 476 (38.4%) | 141 (11.4%) | 147 (11.9%) | 185 (14.9%) | 240 (19.4%) | 51 (4.1%) |
| Use sunglasses | 392 (31.6%) | 143 (11.5%) | 192 (15.5%) | 234 (18.9%) | 241 (19.4%) | 38 (3.1%) |
| Use a hat/cap | 185 (14.9%) | 101 (8.1%) | 217 (17.5%) | 279 (22.5%) | 428 (34.5%) | 30 (2.4%) |
| Wear long sleeves and long pants | 179 (14.4%) | 201 (16.2%) | 335 (27.0%) | 304 (24.5%) | 187 (15.1%) | 34 (2.7%) |
| Avoids midday (12am-4pm) | 41 (3.3%) | 76 (6.1%) | 287 (23.1%) | 393 (31.7%) | 412 (33.2%) | 31 (2.5%) |
| Use of sunscreen SPF ≥15 | 197 (15.9%) | 107 (8.6%) | 215 (17.3%) | 287 (23.1%) | 402 (32.4%) | 32 (2.6%) |
Results are presented as number of patients (%). Based on Troya et al. questionnaire.
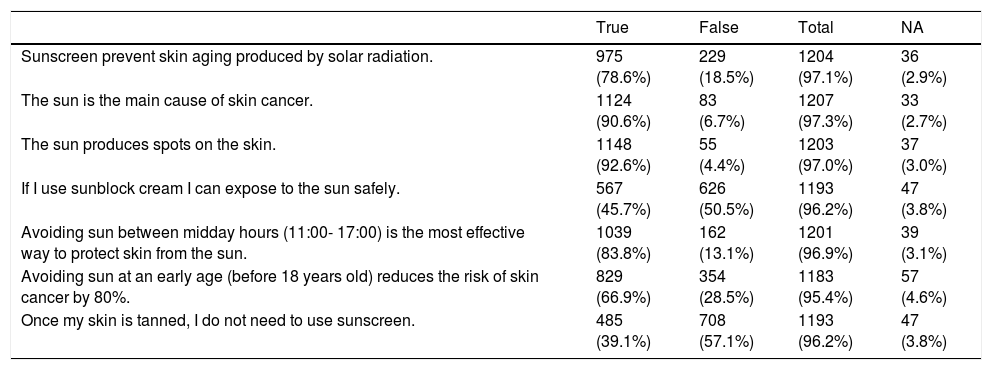
Regarding concerns about AK, self-examination of the lesions was reported in 59.5% of cases, normally once a month (31.5%) or even daily (21.7%), and most of the patients had the conviction that treatment was necessary to improve/heal such lesions (70% very/totally convinced). Globally, the majority of patients answered the correct response in all seven items of the questionnaire of knowledge about sun-exposure. In five of those items success rate in this questionnaire was around 66% to 93% but in two items regarding the safety of sunbathing with sunscreen or being tanned patients scored below 60% of success. Mean global score on the generic questionnaire about sun-exposure knowledge was 5.38 (1.45) out of seven (Table 3).
Questionnaire of general knowledge about sun-exposure.
| True | False | Total | NA | |
|---|---|---|---|---|
| Sunscreen prevent skin aging produced by solar radiation. | 975 (78.6%) | 229 (18.5%) | 1204 (97.1%) | 36 (2.9%) |
| The sun is the main cause of skin cancer. | 1124 (90.6%) | 83 (6.7%) | 1207 (97.3%) | 33 (2.7%) |
| The sun produces spots on the skin. | 1148 (92.6%) | 55 (4.4%) | 1203 (97.0%) | 37 (3.0%) |
| If I use sunblock cream I can expose to the sun safely. | 567 (45.7%) | 626 (50.5%) | 1193 (96.2%) | 47 (3.8%) |
| Avoiding sun between midday hours (11:00- 17:00) is the most effective way to protect skin from the sun. | 1039 (83.8%) | 162 (13.1%) | 1201 (96.9%) | 39 (3.1%) |
| Avoiding sun at an early age (before 18 years old) reduces the risk of skin cancer by 80%. | 829 (66.9%) | 354 (28.5%) | 1183 (95.4%) | 57 (4.6%) |
| Once my skin is tanned, I do not need to use sunscreen. | 485 (39.1%) | 708 (57.1%) | 1193 (96.2%) | 47 (3.8%) |
Note: success appears in bold. Based on Troya et al. questionnaire.
Both dermatologist and patients agreed on the therapeutic plan in 78% of cases. Patients’ mean acceptance was rated as 8.42 (1.35) out of ten. Ninety patients received treatments of a single day duration. In the rest of cases in which therapy was prescribed, 73.8% patients received a therapy that required an application for a week or less.
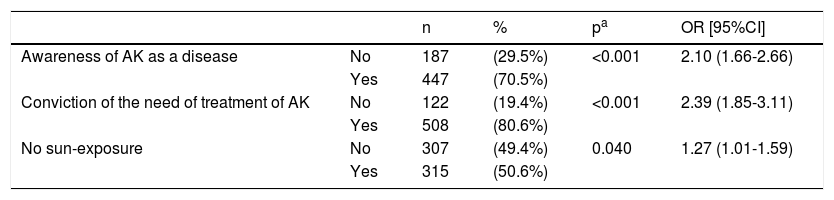
Patients defined as compliant according to the MGT's criteria presented specific differences regarding beliefs and attitudes towards AK and skin care, since they were more likely to consider AK as a disease and to believe that it needs to be treated, and also more aware that they needed to avoid direct sun-exposure (Table 4). These patients also showed higher scores on acceptance of the therapeutic plan when compared with non-compliers (9.70 (1.23) vs 9.11 (1.40); p<0.001). No significant differences were observed between “adherent” and “non-adherent” patients regarding other concerns like “suffering a disease that requires chronic treatment” or their “aesthetic concerns”.
Beliefs and attitudes of patients who show adherence according to MGT.
| n | % | pa | OR [95%CI] | ||
|---|---|---|---|---|---|
| Awareness of AK as a disease | No | 187 | (29.5%) | <0.001 | 2.10 (1.66-2.66) |
| Yes | 447 | (70.5%) | |||
| Conviction of the need of treatment of AK | No | 122 | (19.4%) | <0.001 | 2.39 (1.85-3.11) |
| Yes | 508 | (80.6%) | |||
| No sun-exposure | No | 307 | (49.4%) | 0.040 | 1.27 (1.01-1.59) |
| Yes | 315 | (50.6%) |
Results are presented as numbers of patients and proportions (%). OR [95%CI]: Odds Ratio along with Confidence Intervals at 95%.
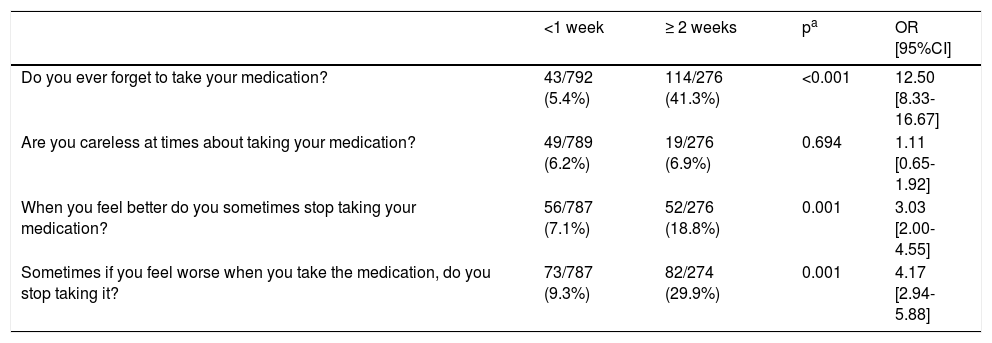
At the end of the study, only 57 patients had not completed treatment as intended, while 55.6% of whole study population achieved complete remission. Global MGT score was 3.55 (0.87) and maximum level of adherence (4 points) was reached by 72.5% of cases (Table 5).
Results for each item of the Morisky-Green test regarding length of treatment.
| <1 week | ≥ 2 weeks | pa | OR [95%CI] | |
|---|---|---|---|---|
| Do you ever forget to take your medication? | 43/792 (5.4%) | 114/276 (41.3%) | <0.001 | 12.50 [8.33-16.67] |
| Are you careless at times about taking your medication? | 49/789 (6.2%) | 19/276 (6.9%) | 0.694 | 1.11 [0.65-1.92] |
| When you feel better do you sometimes stop taking your medication? | 56/787 (7.1%) | 52/276 (18.8%) | 0.001 | 3.03 [2.00-4.55] |
| Sometimes if you feel worse when you take the medication, do you stop taking it? | 73/787 (9.3%) | 82/274 (29.9%) | 0.001 | 4.17 [2.94-5.88] |
| Global Score | ||||
|---|---|---|---|---|
| Non-adherent patients | 138 (17.6%) | 155 (56.6%) | <0.001 | 6.25 [4.55-8.33] |
| Adherent patients | 648 (82.4%) | 119 (43.4%) | ||
| Total | 786 (100%) | 274 (100%) | ||
Results are presented as number of patients and proportion (%). OR [95%CI]: Odds Ratio along with Confidence Intervals at 95%.
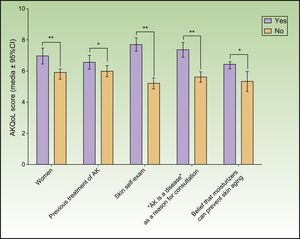
Mean overall AKQoL score at baseline was 6.23 (4.63) and, regarding subscales results, PIQA's population scored a mean of 2.23 (1.95) (out of 9) in “Function” domain, 2.22 (1.95) (out of 9) in “Emotion” domain and 1.29 (1.30) (out of 6) in “Control over life in general” domain. Inferential analysis suggested that patients with higher levels of concern were more likely to show more impaired QoL (Figure 1). Comparison by sex reveals that AK had a greater effect on women's QoL (p <0.001). A higher negative impact on patients’ QoL was observed in cases who perform self-examination of AK lesions (p<0.001), consider AK as a disease (p<0.001) and/or believe that moisturizers can prevent skin aging (p=0.002). Receiving previous treatment for AK was another factor that had a significant impact on QoL (p<0.05) (fig. 1). AK severity assessed by number of lesions did not significantly influence QoL (p=0.194).
Impact of treatment's lengthTo study the impact of treatment's duration we excluded ninety patients that had received a single-day therapy (basically cryotherapy and surgery). Thus, in 93.1 of cases, patients received a specific treatment for more than one day of duration and 79.3% of them applied the medication on 100% of days determined by dermatologist, while 94% showed correct adherence (application of medication on ≥80% of the intended days).
According MGT's assessment, 767 patients (72.4%) met the criteria to be considered adherent to the treatment. Comparison between patients’ length of treatment regarding MGT scores showed that patients with therapies longer than a week were six times less likely to show adherence to treatment. Significant differences in three out of four items of MGT were observed, all of them related with the lack of application of a dose (Table 5).
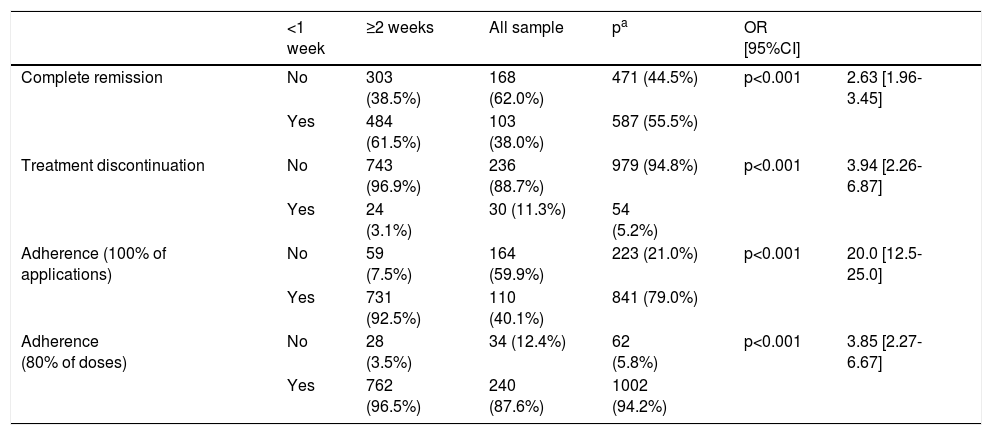
Statistical significant differences were found between those patients receiving treatment that required use/application for less than a week and those with longer treatments in clearance rates and proportion of cases with complete or correct adherence regarding compliance rate with the treatment's application. Furthermore, complete remission was significantly more frequent in patients receiving treatments of <1 week and patients scheduled to receive treatment lasting longer than a week were four times more likely to discontinue (Table 6). There was complete remission in 55.6% of patients against 41.6% of patients which presented partial remission. It also must be noted that there were a very little number of patients (n=4) which discontinued the treatment by self-decision.
Clinical outcomes and adherence according to length of treatment.
| <1 week | ≥2 weeks | All sample | pa | OR [95%CI] | ||
|---|---|---|---|---|---|---|
| Complete remission | No | 303 (38.5%) | 168 (62.0%) | 471 (44.5%) | p<0.001 | 2.63 [1.96-3.45] |
| Yes | 484 (61.5%) | 103 (38.0%) | 587 (55.5%) | |||
| Treatment discontinuation | No | 743 (96.9%) | 236 (88.7%) | 979 (94.8%) | p<0.001 | 3.94 [2.26-6.87] |
| Yes | 24 (3.1%) | 30 (11.3%) | 54 (5.2%) | |||
| Adherence (100% of applications) | No | 59 (7.5%) | 164 (59.9%) | 223 (21.0%) | p<0.001 | 20.0 [12.5-25.0] |
| Yes | 731 (92.5%) | 110 (40.1%) | 841 (79.0%) | |||
| Adherence (80% of doses) | No | 28 (3.5%) | 34 (12.4%) | 62 (5.8%) | p<0.001 | 3.85 [2.27-6.67] |
| Yes | 762 (96.5%) | 240 (87.6%) | 1002 (94.2%) |
Results are presented as number of patients (%). OR [95%CI]: Odds Ratio along with Confidence Intervals at 95%.
This work presents an epidemiological study of a large population with AK in a country characterized by strong recreational sun-exposure habits with the aim to find out the relationship between these and other habits that may also affect relevant clinical variables such patients’ QoL, adherence to treatment and other related parameters. Study's outcomes suggest that concerns about AK are directly proportional to the impact of this disease on patients’ QoL but, on the other hand, patients with more concerns are more likely to show good adherence to AK treatment. Overall, the study population scored significantly higher than the general population evaluated during validation AKQoL scale,18 confirming that the presence of QA affects the patients’ QoL. Another interesting finding was the current picture of a dermatological patient with AK in Spain: a male aged around 73, with phototype II-III, presenting between one and five AK lesions, mainly located on the face and scalp.
Gender distribution and average age of study patients is representative of the population having AK and consistent with previous reports,6,20 with the particularity of a higher proportion of the typically found in Mediterranean countries phototypes (II and III). PIQA study accumulates a broad spectrum of AK lesions, however, as usual in AK, we observed more lesions on the face and scalp than other locations. The high rate of patients with previous treatments may suggest a high frequency of AK relapse and a susceptibility to develop new clinically visible lesions.
Although patients that perform self-examination seem to be aware of the need for treatment, their sun exposure habits do not correspond with this awareness nor the use of photo protective measures. For example, in PIQA study several patients reported sunbathing at the beach or parks within the previous year but few of them used a sunscreen SPF>15 or wore adequate clothing. In this sense, interventions of health education on AK and preventive measures could increase the awareness of the disease, its chronic nature and associated risks with the presence of these lesions, but it seems necessary to pay more attention in remarking the use of photoprotective measures.
Adherence has been strongly associated with efficacy in AK therapy.14 Furthermore, correct compliance with treatment is influenced by medication and patient-related factors.21 Previous research has shown that a wider length of topical treatments for AK negatively impacts on patients’ adherence.9,21,22 For instance, Shergill et al. reported that alternatives intended for application beyond 3 weeks were associated with a 52% of non-complier patients’ rate. Such findings were alike those reported in present study, where such temporal border is even reduced, showing a statistical significant difference (decrease) on adherence from 2 weeks, and also patients with recommended treatments that needed to be applied for less than a week were more likely to comply. As could be expected, it was observed that adherence had a significant impact on the number of patients presenting complete remission of lesions.
Previous to this study, Augustin et al. established a strong significant relation between good clinical outcomes and QoL's improvement, as for the treatment satisfaction.23 In general, our results confirm that AK has a negative impact on patients’ QoL.24 Main factors influencing the AK-related reduction of QoL seem to be the recognition of the pathological nature of these lesions, probably because better knowledge and awareness could drive to increase the level of concern. Differences observed in PIQA study in QoL levels depending on sex might be influenced by cultural aesthetic conceptions, but presented results does not permit to establish a clear relation between them.
The high correlation between lower QoL scores and good adherence suggest that a greater knowledge of AK may have a positive effect on treatment compliance. Therefore, increasing patients’ awareness is the cornerstone of any intervention for the reduction or elimination of these pre-malignant lesions.
It must be considered, given the nature of the observational studies the existence of some limitations and potential biases regarding the use of test based mainly in the patient memories. The main sources of bias that we can find in observational studies can be categorized in selection mechanisms in recruitment of study participants (selection bias), selective recall or inconsistent data collection (information bias), measurement errors confounding, and other errors
In summary, the findings of our study show that AK-related QoL is lower in more concerned patients, and that sex and “awareness of AK as a disease” are important factors which have a particularly strong influence on patients’ QoL. All these concepts are simultaneously associated with adherence to AK treatment, since low QoL are significantly related with higher compliance, and this in turn is connected with better clinical outcomes. In parallel, another important factor to improve adherence to treatment and clinical outcomes is therapy's length, since treatments shorter than one week show statistically significant better results than larger ones. The study demostrate that more concerned patients tend to be more conscious of the need for treatment and have lower QoL, but at same time those patients show better adherence to treatment. The patients’ concerns are related in particular to sex, aesthetic aspects and to the consideration of AK as a disease. Short length of treatment was associated with better adherence and a greater likelihood of achieving complete remission.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Longo I, Serra-Guillén C. Calidad de vida, comportamiento y actitudes hacia la queratosis actínica en España: estudio PIQA. Actas Dermosifiliogr. 2018;109:331–339.