Piezogenic papules are produced by the herniation of adipose tissue through the dermal connective tissue. They develop in up to 60% of the general population1 and are caused by persistent excessive pressure; they are therefore most common in athletes (runners, jumpers, etc.), obese persons, and those who frequently carry heavy weights.2 A high incidence has also been reported in patients with Ehlers-Danlos syndrome due to the disease-related weakness of the collagen.3,4 Presentation is usually as skin-colored papules or nodules on the lateral or posterior surfaces of the heels, although they have been described at less typical sites such as the wrists.5,6 Piezogenic papules are usually asymptomatic and are therefore an uncommon cause of consultation, leading to underestimation of their true prevalence. However, they may occasionally give rise to pain, typically due to the continuous friction with footwear.2,3
The diagnosis of piezogenic papules is above all clinical, though atypical presentations may lead to a need to perform biopsy for histologic confirmation of the suspected diagnosis.1 High-frequency ultrasound, ever more widely employed in dermatology,7,8 can be used to support the clinical diagnosis.
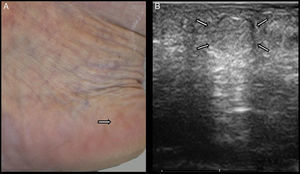
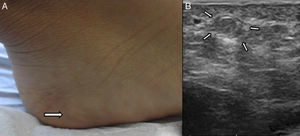
We present 2 cases, one of an obese 52-year-old woman with no other history of interest (Fig. 1A) and the other of a child aged 13 years who regularly practiced aikido (Fig. 2A). These cases help to illustrate the potential usefulness of ultrasound as a diagnostic tool for this condition. Both patients presented asymptomatic skin-colored papules of soft consistency on the medial surface of both heels. The papules measured 0.5cm in diameter and became more prominent when the patients stood up. Despite the characteristic clinical presentation, ultrasound was performed to characterize the lesions sonographically. The ultrasound device (Esaote, MyLabClass C, Genoa, Italy) had a variable-frequency linear array transducer; the frequency for the test was 18MHz, with a lateral resolution of 240μm. The patients were examined in a sitting position, with the knees flexed and the soles of their feet resting on the examination couch, rocking the body weight onto the feet to make the alteration more evident. In both cases, an area was observed that was isoechoic with the subcutaneous cellular tissue but was surrounded by the reticular dermis, producing posterior acoustic enhancement (Figs. 1B and 2B). No abnormal vascularization was observed in color Doppler mode. The ultrasound findings helped to confirm the suspected diagnosis of piezogenic papules. No further diagnostic tests or treatment were considered necessary.
A, Clinical photograph of piezogenic papules in a 52-year-old woman, visible even without weightbearing. Small, round, skin-colored papules/nodules are present on the medial surface of the heel. B, Ultrasound image of a piezogenic papule. An area isoechoic with the underlying subcutaneous cellular tissue is observed within the reticular dermis. There is slight thickening of the dermis.
A, Clinical photograph of piezogenic papules in a 13-year-old girl. Small, round, skin-colored papules/nodules are visible on the medial surface of the heel. B, Ultrasound image of a piezogenic papule. A round hypoechoic area is observed in the dermis. This corresponds to a fat lobule surrounded by the reticular dermis.
These examples illustrate the possibility of using high-frequency ultrasound as an additional test for the diagnosis of piezogenic papules.
Cho et al.9 described similar ultrasound findings in 4 patients. As in the cases described by those authors, ultrasound study of the regions with a clinical suspicion of piezogenic papules in our patients revealed areas within the reticular dermis that were isoechoic with the subcutaneous cellular tissue. Cho et al. explained that the ultrasound image may represent rupture of the interlobular septa adjacent to the reticular dermis and the coalescence of the most superficial fat lobules. In our patients, in contrast to the description by Cho et al., we observed posterior enhancement that could have been due to different ultrasound transmission by this area of subcutaneous cellular tissue compared with adjacent areas of the dermis. It should be noted that the device used by Cho et al. operated at a variable frequency of 5-12MHz whereas, in our patients, we used a device with a linear array with a variable frequency of 16 to 22MHz.
The clear delimitation of the lesion and the absence of abnormal vascularization within the lesions support their benign nature.10 The differential diagnosis should include other benign dermal or subdermal lesions such as lipoma, neurofibroma, and even benign vascular tumors such as a glomus tumor at an atypical site. On ultrasound, lipoma appears as a well-defined, elongated, hypo- or isoechoic area in the hypodermis, with its long axis parallel to the skin surface; it may contain hyperechoic striate lines, which represent the septa.11,12 Neurofibroma is described sonographically as a well or ill-defined nodular or pseudonodular lesion that is homogeneously hypoechoic or that may contain hyperechoic areas within a hypo- or anechoic mass, with a variable degree of vascularization.13 Plexiform neurofibromas, however, appear as hypoechoic and hypovascular tracts that follow the paths of nerves.13 Glomus tumor is seen as a small, solid, well-defined, hypoechoic nodule in the dermis, with abundant blood vessels visible on color Doppler mode.14
Apart from the study by Cho et al., we have found no other articles in the literature that have characterized piezogenic papules using high-frequency ultrasound. We therefore consider that studies with a larger number of patients could be of interest to validate the ultrasound patterns and thus enable us to improve the sensitivity and specificity of the ultrasound diagnosis of dermal and subdermal lesions.
Please cite this article as: Rodríguez-Bandera AI, Alfageme Roldán F, Hospital-Gil M, de Lucas Laguna R. Utilidad de la ecografía de alta frecuencia en el diagnóstico de las pápulas piezogénicas. Actas Dermosifiliogr. 2015;106:591–593.