Among the cutaneous adverse effects associated with drugs used in clinical practice, those caused by antibiotics are particularly frequent. Examples include minocycline-induced pigmentary changes of the skin or mucous membranes. However, these alterations are rarely associated with the use of other antibiotics. We report the uncommon case of a patient who developed blackish lesions on the lower limbs after beginning levofloxacin treatment.
Case DescriptionA 72-year-old man with a previous biopsy-confirmed diagnosis of pigmented purpuric dermatosis (PPD) of the legs was seen for darkening of the skin of the lower limbs that had begun 10 months earlier. Two years earlier, the patient had undergone surgery for implantation of a prosthesis in the right shoulder. He had been receiving levofloxacin treatment for several months to treat an infection of the prosthesis. He reported that the skin discoloration appeared a few weeks after beginning levofloxacin treatment. Physical examination revealed very striking diffuse, blackish-gray pigmentation distributed bilaterally and symmetrically on the anterolateral aspects of the legs, from the knees to the toes, sparing the soles (Fig. 1). The mucous membranes were unaffected. The distal pulse was preserved and there were no other signs of ischemia.
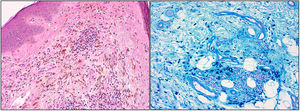
A biopsy showed extensive deposition in the superficial and middle dermis of macrophages containing brown granular refractive cytoplasm, and a focal lymphocytic inflammatory infiltrate containing extravasated red blood cells. Perls staining was strongly positive inside the macrophages (Fig. 2A, B). Von Kossa and Fontana Masson staining were negative.
Levofloxacin treatment was suspended, resulting in a striking improvement in the skin pigmentation. Within 4 months, the patient's skin color had returned to normal (Fig. 3).
DiscussionQuinolone treatment has been associated with certain cutaneous adverse effects. Specifically, levofloxacin can cause phototoxicity, toxic epidermal necrolysis,1 drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome,2 fixed drug eruption,3 and leukocytoclastic vasculitis,4 among other conditions. However, no association between pigmentary disorders and levofloxacin use has been previously reported.
To date, lesions similar to those of our patient have been attributed in almost all cases to minocycline, which causes pigmentation disorders in up to 50% of patients undergoing prolonged treatment.5,6 We have found only 2 descriptions of patients with blackish-blue lesions similar to those of our patient caused by levofloxacin. In one of those patients, the backs of the hands as well as the legs were affected. In both cases, the histological findings corresponded to those of our patient, and the lesions improved after discontinuation of levofloxacin therapy.7,8 A third report describes a case almost identical to ours that was caused by pefloxacin treatment and in which subsequent exposure to norfloxacin resulted in lesion recurrence.9
Our patient had been previously diagnosed with PPD, which worsened after beginning levofloxacin treatment. We have found no descriptions in the literature of PPD secondary to treatment with levofloxacin or other quinolones that could explain this disimprovement. Furthermore, Perls staining of the biopsy sample revealed positive staining exclusively inside macrophages, and not in the stroma, as would be expected in PPD. Therefore, we propose that the patient's condition was independent of the underlying PPD and mainly due to levofloxacin treatment.
We believe that this case is of particular interest because it resembles, but is distinct from, pigmentation that typically occurs following minocycline treatment. The mechanism by which these cutaneous pigmentary alterations occur is unclear. In the case of minocycline-associated pigmentation the nature of the pigmented particles within the macrophages is unknown. Depending on the type of pigmentation, of which 3 distinct forms are described, histology shows dermal granules that are either free or located inside macrophages and contain iron and melanin, as revealed by Perls and Masson Fontana staining, respectively. Positive von Kossa staining, indicating the presence of calcium compounds, has been described in some cases.10 Proposed explanations to account for the presence of these pigmented particles include the deposition of different types of drug metabolites, the presence of iron chelators within melanophages, and increases in the production of intracellular melanin.7 In the case of levofloxacin-induced pigmentation it is difficult to draw conclusions owing to the paucity of cases described. Perls staining was positive in our patient and in the 2 previously described cases. Masson Fontana staining was also positive in the case described by Garval and coworkers,7 but was negative in our patient, as was von Kossa staining, which was not described in either of the 2 published case reports. The study of additional similar cases would help to further our understanding of this unusual entity.
ConclusionWe report a rare case of striking cutaneous pigmentation caused by levofloxacin treatment. This case underscores the importance of taking changes in the patient's usual medication into account when examining possible skin lesions.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors thank Dr. Ángel Fernández Flores for his generosity and his helpful contribution to this case.
Please cite this article as: Castellanos-González M, González Morales ML, González-Granda Villalobos J. Levofloxacin-Induced Hyperpigmentation. Actas Dermosifiliogr. 2019;110:700–701.