The term cutis verticis gyrata (CVG) describes the finding of folds and creases on the top of the scalp, forming patterns reminiscent of those of the surface of the brain.1
We report the case of a 25-year-old man who visited our department with pruritis on the scalp that had appeared several months earlier. The patient's past history included immunoglobulin-A (IgA) deficiency, bilateral sensorineural hearing loss, and bilateral diffuse cataracts. Analytical tests and cranial CT scans performed during childhood were normal, and congenital rubella and Alport syndrome were ruled out. The patient's intellectual development and social adaptation were normal.
Physical examination at our department revealed hypertrophy and formation of anteroposterior folds on the scalp, forming furrows and ridges (Fig. 1). The patient presented no desquamation, hair loss, or other skin lesions.
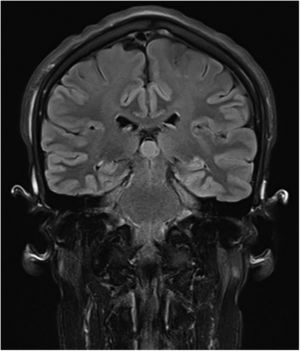
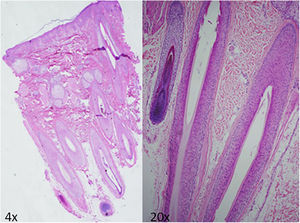
Cranial magnetic resonance imaging revealed slight undulation of the extracranial soft tissue, with no associated involvement of the bone or intracranial tissue (Fig. 2). A skin biopsy of the scalp revealed follicular hypertrophia and hyperplasia, with no other histologic findings of interest (Fig. 3). Blood tests (blood count, glycemia, lipid, hepatic, renal, and thyroid profiles, cortisol, parathyroid hormone, and acromegaly screening) were normal. In light of these findings, the patient was diagnosed with primary nonessential CVG.
Our patient presented intense pruritis, which had previously been treated with oral antihistamines and topical antipruritics, with no response. Treatment with capsaicin gel 0.075% was instated but the patient's condition worsened; oral gabapentin was then instated with no improvement, and both treatments were therefore suspended. Finally, amitriptyline was prescribed at a dosage of 10mg per day, and the patient remains asymptomatic to date (5 months).
CVG is a rare morphologic syndrome that presents with hypertrophy and folding of the scalp. Incidence in the general population is difficult to estimate, as the disease is generally asymptomatic.
The primary form has no known cause and may occur in isolation (primary essential CVG) or in association with other neurologic (intellectual disability, deafness, microcephaly, or epilepsy) and/or ophthalmologic abnormalities (cataracts, strabismus, blindness, or retinitis pigmentosa).1,2 It is more common in males,1 with onset usually occurring during puberty, and is usually distributed symmetrically, typically affecting the vertex and occipital region,2 in the form of anteroposterior furrows and ridges that give it the appearance of the surface of the brain.
Secondary CVG is due to the abnormality in the scalp caused by other diseases such as acromegaly, myxedema, fragile X syndrome, Klinefelter syndrome, tuberous sclerosis, psoriasis, eczema, Darier disease, amyloid deposition, extensive nevus or hamartoma, leukemia, Ehlers-Danlos syndrome, or trauma.1–3
Study of the patient should initially be guided by past history, the physical examination and the biopsy of the affected area, and associated abnormalities and the diseases that cause secondary forms should be ruled out using different tests and imaging studies.1
A typical biopsy of the primary form will reveal hypertrophy and hyperplasia of adnexal structures and increased dermal collagen in skin with no other histologic abnormalities.2 Secondary CVG shows abnormalities characteristic of the underlying etiology.
As well as the above-mentioned diseases, the differential diagnosis includes pachydermoperiostosis, Beare-Stevenson cutis gyrata syndrome, and lipedematous scalp. Pachydermoperiostosis is characterized by pachyderma, periostosis, and clubbing of the fingers, and may be associated with CVG.4 Beare-Stevenson cutis gyrata syndrome typically presents with craniosynostosis, prominent umbilical cord stump, or acanthosis nigrans, and sometimes presents CVG as a phenotypic trait.5 Unlike CVG, lipedematous scalp courses with thickening of the scalp, but this is caused by hyperplasia of the subcutaneous tissue due to proliferation of adipocytes.6
Primary CVG is asymptomatic in most cases. If it poses an aesthetic problem, surgical treatment may be performed and different techniques such as partial excision, use of tissue expanders and plasties,7 or fold subcision8 have been reported. In secondary CVG, the causal disease is treated.
Higher prevalence of skin disease such as atopic dermatitis has been reported in contexts of IgA deficiency. In the last count, our patient showed IgA levels of 76mg/dL (normal range, 108-325mg/dL) and had no history or clinical signs of atopic dermatitis or other skin disease that explained the pruritis. Furthermore, the IgA deficiency was diagnosed in infancy and the pruritis, located exclusively in the scalp, began when the patient was 25 years old, coinciding with when he first noticed the skin folds at that site.
To date, we have found no cases of pruritic CVG in the literature. We therefore based the treatment of this patient on that described for dysesthesia of the scalp.9 The use of oral antidepressants in patients with chronic pruritis that does not respond to oral antihistamines or topical treatment has been widely reported. While randomized clinical trials are needed, the literature contains case series and open clinical trials in which these drugs have been efficacious.10 Our case joins this group of patients, with an atypical form of CVG that courses with pruritis and responds to amitriptyline – something we have not found in the literature to date.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tomás-Velázquez A, Moreno-Artero E, Abengózar M, Palacios-Álvarez I. Cutis verticis gyrata primario no esencial pruriginoso. Actas Dermosifiliogr. 2019;110:702–704.