Biologic therapies are increasingly used to treat many inflammatory conditions, including skin diseases. Adverse effects include infections, some of which are potentially serious.1
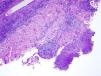
A 53-year-old male livestock worker with psoriatic arthritis, for which he had been treated with leflunomide (5 years) and certolizumab (2 years), presented with an asymptomatic lesion on the wrist that had appeared 15 days earlier and had not responded to a 1-week course of oral clarithromycin (500mg/12 h) and topical fusidic acid therapy. The patient reported neither fever nor systemic symptoms. Physical examination revealed an indurated, erythematous-violaceous nodule (2cm in diameter) with a central crust on the dorsum of the left wrist (Fig. 1). A swab sample was collected from the lesion surface for culture and a skin biopsy was taken for culture and histopathology.
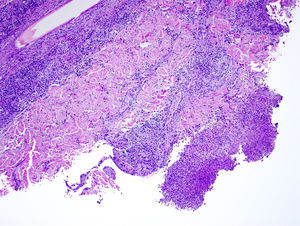
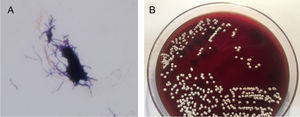
The biopsy showed a superficial and deep predominantly neutrophilic inflammatory infiltrate that formed focal dermal abscesses. No nuclear pseudoinclusions were observed. Periodic acid-Schiff (PAS) and silver staining were negative (Fig. 2). The swab culture was negative, but Nocardia brasiliensis resistant to clarithromycin and sensitive to trimethoprim/sulfamethoxazole was isolated from the skin biopsy culture (Fig. 3). A basic battery of tests and pulmonary and brain computed tomography (CT) revealed no findings of note. The patient was diagnosed with localized primary cutaneous nocardiosis. After discontinuing certolizumab treatment, he began treatment with trimethoprim/sulfamethoxazole (80mg/12h and 400mg/12h, respectively), which resulted in complete lesion resolution in 6 months.
Nocardiosis is a rare infection that most often affects immunocompromised patients, and is considered an emerging infectious disease by some authors.2,3 Cutaneous nocardiosis accounts for up to 25% of cases and can lead to disseminated disease.4 It is caused by direct inoculation, mainly by N brasiliensis. The localized cutaneous form can be indistinguishable from other pyodermas and in one third of cases evolves to a lymphocutaneous form, with formation of nodules along the lymphatic pathway.5 The differential diagnosis includes bacterial (erysipeloid, tularemia, and anthrax), fungal (sporotrichosis), and viral (Orf and milker's nodules) infections, as well as atypical mycobacterial infections and leishmaniasis. A secondary form of nocardiosis, caused by hematogenous seeding from another focus, can resemble the primary form and can cause significant morbidity and mortality. Diagnosis is established by culture of samples acquired by invasive methods such as biopsy or aspiration of pus. In cases of clinical suspicion of nocardiosis the microbiologist should be notified in advance to ensure culture of the sample in the appropriate medium.6 Because sensitivity profiles differ between species, it is advisable to perform an antibiogram.7 Histopathology reveals nonspecific changes and silver staining occasionally enables visualization of the microorganisms.5,6 In patients with cutaneous nocardiosis, especially immunocompromised patients, systemic disease should be ruled out by pulmonary and cerebral CT.6
Tumor necrosis factor α (TNF-α) plays an important role in immunity against intracellular pathogens such as Nocardia species.2 Of the 11 reported cases of nocardiosis in patients receiving anti-TNF therapy, 3 involved patients with primary cutaneous nocardiosis2–4,8 and none were associated with certolizumab treatment. Singh and coworkers described a case of cutaneous nocardiosis in a 45-year-old patient with Crohn disease who was being treated with prednisone and infliximab.8 Ali et al reported the case of a 61-year-old Crohn disease patient who was being treated with infliximab.2 In both cases, the causative species could not be identified. Fabre et al described the case of a 70-year-old rheumatoid arthritis patient who was being treated with infliximab, methotrexate, and corticosteroids, and who developed primary cutaneous nocardiosis due to Nocardia otitidiscaviarum.4 In none of the aforementioned cases were systemic symptoms or disseminated disease observed. All patients progressed favorably after discontinuing anti-TNF treatment and beginning treatment with trimethoprim/sulfamethoxazole2,8 or ofloxacin and clindamycin.4 Although leflunomide has been associated with the development of intracellular pathogen infections, to our knowledge no cases of leflunomide-associated nocardiosis have been reported. Compared with other disease-modifying antirheumatic drugs, anti-TNF therapy is associated with an increased risk of skin and soft tissue infections.9 Based on this association and the sequence of clinical events in the current case, we believe that certolizumab was the main determinant of our patient's condition.
While there is currently insufficient evidence to recommend a specific drug regimen and treatment duration, trimethoprim/sulfamethoxazole therapy for 3 to 12 months is considered the treatment of choice, depending on the patient's immune status, and desensitization therapy is recommended in cases of allergy.3 Localized forms of nocardiosis can be surgically removed to shorten the treatment duration.6 Immunosuppressive drug treatment should be withdrawn or continued at the minimum dose. A lack of improvement after 2 weeks can indicate resistance, poor tissue penetration, or the need for surgical drainage. It should be noted that clinical suspicion is fundamental for early diagnosis and treatment, and for early withdrawal of anti-TNF therapy.3,6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors thank Dr. Daniel Tena Gómez (Microbiology Department), Dr. Itziar Eraña Tomás and Dr. Jesús Cuevas Santos (Pathological Anatomy Department), and Dr. Esteban Martín Echevarría (Internal Medicine Department) of the University Hospital of Guadalajara for their assistance with the diagnosis and the writing of the manuscript.
Please cite this article as: Gil Redondo R, Melgar Molero V, Martín Fuentes A, de Eusebio Murillo E. Nocardiosis cutánea primaria en un paciente en tratamiento con certolizumab. Actas Dermosifiliogr. 2019;110:698–699.