Cutaneous sarcomas constitute less than 1% of superficial soft tissue neoplasms. Leiomyosarcomas (LMSs), which account for between 3% and 6.5% of cutaneous sarcomas, are classified as dermal (derived from the hair erector muscle) or subcutaneous (derived from the smooth muscle of vessel walls).1 This classification has prognostic relevance, as dermal LMS has a more favorable clinical course and outcome; metastasis occurs in 5% to 10% of dermal cases as compared with 30% to 40% of subcutaneous cases.2
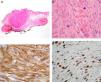
We report the case of a 63-year-old man with a medical history of hypertension, hyperuricemia, and dilated cardiomyopathy, who presented with an asymptomatic and progressively growing nodular lesion in the ciliary region of the left eye that had appeared 6 months previously (Fig. 1). Physical examination revealed a raised, indurated, and erythematous lesion, with destruction of hair follicles, that was surrounded by a halo of firm, edematous skin. Dermoscopy showed a homogeneous brown pattern with no other notable features. Based on a clinical diagnosis of basal cell carcinoma the lesion was excised and the surgical defect reconstructed with a transposition flap.
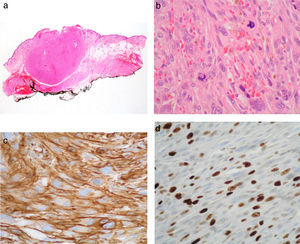
Histologic examination revealed a malignant mesenchymal neoplasm of 7mm in diameter, with expansive borders. The tumor occupied the entire thickness of the dermis, extended into the hypodermis, and was located within 1mm of the deep resection margin (Fig. 2). The tumor was composed of spindle cells arranged in intersecting fascicles. The nuclei were atypical, pleomorphic, elongated, and had rounded edges. The mitotic index was 15 mitoses per 10 high power fields (HPF). Immunohistochemistry was positive for muscle markers (smooth muscle actin, desmin, caldesmon) and negative for S-100 and CD34. The Ki-67 proliferative index was 20%. A diagnosis of dermal leiomyosarcoma with infiltration of the hypodermis was established. No metastasis was detected in the staging study. Ten months after surgery, the patient remains free of disease.
A, Panoramic microscopic image shows a neoplasm with an expansive growth pattern, which does not affect the resection margin (hematoxylin-eosin, original magnification ×4). B, The neoplasm is composed of spindle cells arranged in fascicles with marked atypia and abundant mitotic figures (hematoxylin-eosin, original magnification ×40). C, Expression of smooth muscle actin (Papanicolaou, original magnification ×40). D, The proliferative index (Papanicolaou, Ki-67) is 20%.
LMSs are rare cutaneous neoplasms that occur in middle-aged men, some of whom may have a medical history of trauma. The most common site of LMS is the flexor surfaces of the lower extremities, followed by the scalp and trunk. Facial localization is rare.
While LMSs that are confined to the dermis do not usually metastasize,3 the rate of recurrence is over 30%. Deeper tumors may metastasize in up to 30% to 40% of cases, especially to the lungs.4 In general, LMSs are asymptomatic and grow slowly. In rare cases these tumors can cause pain, itching, tenderness, or bleeding.3 They usually appear as a solitary, firm, raised lesion of between 0.5cm and 3cm, sometimes with ulceration.
Histologically, LMS tumors have infiltrative borders, consisting of spindle cells embedded in a collagenous stroma. They sometimes show a fascicular arrangement and may be accompanied by a peritumoral or intratumoral lymphocytic inflammatory infiltrate.5 Two growth patterns have been described: a nodular pattern, with high cellularity, nuclear atypia, and mitoses, and a diffuse pattern, with low cellularity and proliferative activity.
The malignancy criteria established by the World Health Organization include high cellularity, nuclear atypia, and at least 1 mitosis per 10HPF.6
Clinical suspicion of LMS is uncommon.3 Histopathological examination is usually necessary for diagnosis, as physical examination reveals no specific findings that facilitate the identification of LMS. The differential diagnosis includes other soft-tissue spindle-cell tumors (e.g., fibrosarcoma, malignant histiocytoma, dermatofibroma, atypical fibroxanthoma, spindle cell melanoma, sarcomatoid carcinoma, leiomyoma) and immunohistochemical techniques are required for proper grading (Table 1).2,7,8 A recent study described the usefulness of phosphohistone H3, an immunohistochemical marker of mitosis, in distinguishing between leiomyosarcoma and leiomyoma.7
Immunohistochemistry of Cutaneous Spindle-Cell Tumors.
| MarkerTumor | CD10 | CD34 | Vimentin | Desmin | Smooth Muscle Actin | S-100 Protein | HMB-45 | HMW Cytokeratins |
| DFSP | - | + | + | - | - | - | - | - |
| AFX | + | -/+ | + | - | -/+ | - | - | - |
| MFH | - | -/+ | + | - | -/+ | - | - | - |
| SCSCC | - | - | +/- | - | - | - | - | + |
| LMS | - | -/+ | + | + | + | - | - | -/+ |
| DM | -/+ | - | -/+ | -/+ | -/+ | + | - | -/+ |
| AS | + | + | + | - | - | - | - | +/- |
Abbreviations: AFX, atypical fibroxanthoma; AS, angiosarcoma; DFSP, dermatofibrosarcoma protuberans; DM, desmoplastic melanoma; HMW, high molecular-weight; LMS, leiomyosarcoma; MFH, malignant fibrous histiocytoma; SCSCC, spindle-cell squamous cell carcinoma.
In 2003 Hornick and Fletcher5 proposed the term atypical smooth muscle tumors for cutaneous smooth muscle tumors with mitotic figures and cellular atypia, and proposed reserving the term leiomyosarcoma for tumors affecting subcutaneous tissue. In 2011, Kraft and Fletcher9 published an analysis of 84 cases of primary LMS (atypical smooth muscle tumors); 61 (72.9%) of these were limited to the dermis and 23 (27.1%) involved superficial extension into the subcutaneous tissue. No metastasis was detected in any of these cases, with a mean follow-up of 51 months. Given the low (or absent) risk of metastasis, those authors concluded that it was inappropriate to classify this lesion as a sarcoma, preferring the term atypical intradermal smooth muscle neoplasm. We disagree with this view, as other histologically malignant cutaneous neoplasms (e.g., dermatofibrosarcoma protuberans) have a more benign biological behavior, with very low metastatic potential in most cases, and thus should be referred to using the original terminology.10
The treatment for cutaneous LMS is excision with wide margins (at least 3-5cm). These tumors show a poor response to chemotherapy and radiation therapy, although the latter may be indicated for high-grade tumors of more than 5cm in diameter, in cases of excision of recurrent tumors, or after surgery with inadequate margins.
Please cite this article as: Lozano Salazar A, Márquez García A, Ortega Medina I, Ríos-Martín J. Leiomiosarcoma dérmico en la cola de la ceja izquierda. Actas Dermosifiliogr. 2014;105:879–882.