Inflammatory skin diseases are common in patients infected by the human immunodeficiency virus (HIV), especially in those who are severely immunocompromised. In addition, there is a marked association between inflammatory skin diseases and aggressive lymphomas, particularly in cases of extranodal disease. Although most cases with this association are B-cell lymphomas, the most common primary cutaneous lymphomas are cutaneous T-cell tumors.
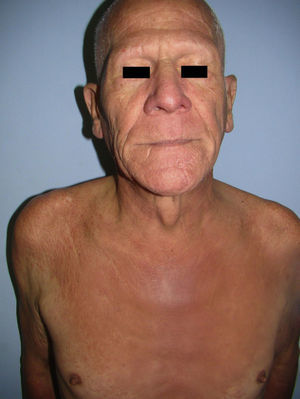
A 60-year-old man with mild chronic obstructive pulmonary disease for which he occasionally used an inhaler presented with intensely pruritic skin lesions on exposed areas that had first appeared 8 months previously. He also reported generalized hair loss, weight loss, and a sensation of unmeasured temperature variability. Physical examination revealed generalized lichenified and erythematous plaques, together with alopecia universalis and signs of inflammatory infiltration on the face, especially above the eyebrows, giving him a leonine appearance (Fig. 1). Palmoplantar involvement, lymphadenopathy, and visceromegaly were not observed.
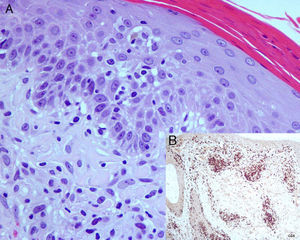
At low-magnification biopsy specimens taken from lesions on the scalp and upper right arm revealed a moderate perivascular inflammatory infiltrate in the superficial dermis, with focal involvement of the epidermis and hair follicles. Increased magnification revealed that the superficial dermal inflammatory infiltrate was composed of lymphocytes with enlarged, irregular nuclei and involving points of mild epidermal spongiosis. Immunohistochemical staining with anti-CD3 revealed mainly CD8 positivity and scant CD4+ cells. Staining for CD30 was negative (Fig. 2). Testing to detect clonal rearrangement of the immunoglobulin heavy chain gene (JH segment) and T-γ and T-β receptor gene was negative.
A, Presence of a superficial dermal inflammatory infiltrate composed of lymphocytes with enlarged, irregular nuclei and involving points of mild epidermal spongiosis (hematoxylin-eosin, original magnification ×400). B, Immunohistochemistry revealed positivity with anti-CD8 antibody (Novocastra streptavidin-biotin-diaminobenzidine, original magnification ×100).
The patient was admitted for evaluation of a constitutional syndrome. The most notable findings in the laboratory workup were elevated peripheral eosinophil counts and frequency (570/μL, 20.9%) and a high lactate dehydrogenase concentration (877 U/L). Serology for HIV was positive, whereas tests for other entities (syphilis, hepatitis B virus, hepatitis C virus, cytomegalovirus, and Epstein-Barr virus) and tumor markers were negative. Cytometry revealed a low CD4:CD8 ratio (0.15; reference range, 1-4), reduced absolute CD4 lymphocyte count (197/μL), increased absolute CD8 lymphocyte count (1291/μL), and a low viral load (1293/mL). Computed tomography of the chest revealed centrilobular emphysema but no masses or enlarged nodes. Abdominal ultrasound revealed a hypertrophic prostate with an adenomatous appearance. The electrocardiogram revealed mild tricuspid insufficiency. No findings of interest were observed in the computed tomography of the head.
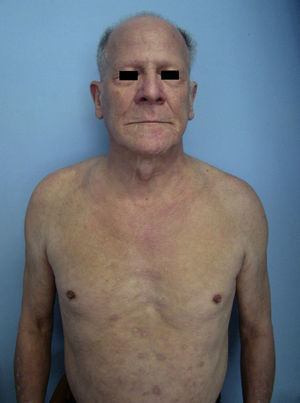
These data confirmed a diagnosis of HIV-associated atypical cutaneous CD8+ T-cell infiltrate or cutaneous CD8+ pseudolymphoma. After 3 months of systemic antiretroviral therapy (ritonavir, atazanavir, emtricitabine, and tenofovir) and tapered oral prednisolone (starting at 45mg/d), the patient's progress was good, with a decrease in the number of lesions, resolution of pruritus, and weight gain. In addition, the hair on his scalp and eyebrows began to grow back again (Fig. 3).
Mucocutaneous disorders are very common in HIV-infected patients. Lymphomas are the second most common HIV-associated malignancy after Kaposi sarcoma. Most cases involve non-Hodgkin lymphoma, with a higher incidence of aggressive B-cell subtypes and extranodal disease,1,2 although cases of cutaneous T-cell lymphoma have also been reported.1,3 HIV-associated polyclonal lymphoproliferative disorders have recently been reported1,4,5; however, these can mimic cutaneous T-cell lymphoma both clinically and histologically, as occurred in the case we report.1–7 Cutaneous CD8+ pseudolymphoma is uncommon in HIV-infected patients and its pathogenesis poorly understood.2,6 It usually presents as extensive plaques or erythroderma1,2,4,6,8 and is often associated with eosinophilia.6 Histology generally reveals a massive dermal infiltrate composed of CD8+ T cells, with or without involvement of the epidermis, and negative results in the clonality study.2–4,6
The literature contains few cases of HIV-associated cutaneous CD8+ pseudolymphoma,1–4,6,7 which usually appears in later stages of the disease and is associated with severe CD4 lymphopenia.1,2,6 The disease is usually treated with systemic corticosteroids, although a favorable response to antiretroviral therapy has been reported.6
In our patient, diagnosis was based on the correlation between clinical and pathology findings, including clinical course, response to antiretroviral therapy, and the results of immunohistochemistry and the molecular biology techniques used for the clonality study.
In conclusion, this diagnosis should be considered when an HIV-infected patient has intensely pruritic skin infiltration, alopecia universalis, weight loss, and eosinophilia. Nevertheless, differential diagnosis should include cutaneous T-cell lymphoma, primary hypereosinophilic syndrome (>1500/μL in peripheral blood for more than 6 months with no other apparent explanation), toxicoderma, atopic dermatitis, contact dermatitis, parasitic infestation, and other HIV-associated skin diseases, such as papuloerythroderma of Ofuji.
Please cite this article as:Fernández-Morano T, Aguilar-Bernier M, del Boz J, Fúnez-Liébana R. Infiltración cutánea por linfocitos T CD8+ asociada a virus de la inmunodeficiencia humana. Actas Dermosifiliogr.2012;103:638-640.