Connective tissue nevus is a type of dermal hamartoma with a variable clinical presentation. This condition generally appears on the trunk or limbs as flesh-colored, yellowish, or brownish plaques with a marbled surface. Its most typical presentations include the orange-peel skin associated with tuberous sclerosis or cobblestone plaques. Connective tissue nevus is characterized by excess collagen or altered elastic fibers. Diagnosis is based on the correlation of clinical and pathological findings, and it is essential to identify variants that are potentially associated with extracutaneous manifestations. Zosteriform connective tissue nevus is an extremely rare variant, with only 5 cases reported to date.
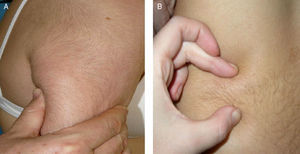
We present the case of a 14-year-old girl with no past history of interest who came to our clinic with an indurated area on her right upper arm that first appeared when she was 6 months old. The lesion initially measured 1cm and had gradually increased in size until it involved the whole deltoid area of that arm. The only concomitant symptom was difficulty raising her arms. Physical examination revealed a poorly defined indurated plaque measuring 7×13cm that extended from the deltoid area to the outer aspect of the right upper arm. The plaque was firm in consistency, had a cobblestone appearance, and was adherent to the deeper layers of the skin, with no alteration to adnexa or changes in the skin surface. She presented a second, similar plaque measuring 8×2cm on her lower back (Fig. 1A and Fig. 1B).
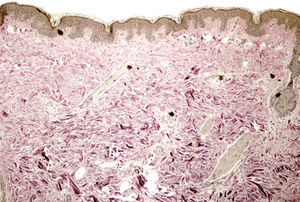
There were no significant findings on hematoxylin-eosin staining of a biopsy specimen of the lesion on the arm with the inclusion of subcutaneous tissue; however, staining for elastic fibers revealed a conserved epidermis and marked reduction and fragmentation of elastic fibers in the reticular dermis (Fig. 2). No accompanying inflammatory infiltrate was observed. The results of imaging tests (ultrasound, magnetic resonance, and Doppler ultrasound) were normal. No significant findings were detected in the complete blood count, biochemistry with liver and kidney function tests, or coagulation studies, and the results of an assessment in the cardiology department were unremarkable. After physiotherapy, physical examination revealed reduced infiltration, even though the lesions had extended to the elbow and onto the forearm.
The term connective tissue nevus was first mentioned by Lewandowsky in 1921, although it was not accepted until the review by Gutmann1 in 1926. Connective tissue nevus is considered a hamartoma of connective tissue (collagen or elastic tissue) that takes the form of tumor-like dermal lesions. Attempts have been made to classify the lesions according to histologic criteria, clinical criteria, or both. One of the most widely accepted classifications is that of Pierard and Lapiere, which divides connective tissue nevi into 2 types—reticular and adventitial—according their clinical and histopathological presentation. Zosteriform nevus is an unusual form of reticular connective tissue nevus that is diagnosed according to its clinical distribution. It was first described by Steiner2 in 1944. Since then, only 5 cases have been published (Table 1); 3 of those involved multiple lesions.
Cases of Zosteriform Connective Tissue Nevus.
| Steiner2 | Kozminsky et al.4 | Yeh et al.5 | Amjadi et al.6 | Brazelli et al.7 | |
| 5 y | 23 y | 3 y | 25 y | 8 y | |
| Female | Female | Male | Female | Female | |
| Single plaque | Several plaques | Single plaque | Forty nodules | Several plaques | |
| Site | Right thorax and back | Dermatomes C6−T1 | Right flank | Right lumbar region and upper part of right buttock | Lumbosacral region and proximal right leg |
| Clinical course | a | Since 7 years of age | Since birth | Since 6 years of age | |
| Concomitant symptoms and course | a | None | None | Isolated fibroma in right axilla | None |
| Stable | Stable over time with no increase in size | Progressive growth until 19 years of age. Some lesions coalesced to form plaques. Stable since then | |||
| Pathology | a | Fragmented elastic fibers in the mid dermis. Trichrome staining did not reveal collagen abnormalities | Fragmented elastic fibers in the mid dermis. No collagen abnormalities | Excess collagen. Remaining connective tissue normal. No other significant findings | Thickening and sclerosis of the collagen fibers in the superficial, mid, and deep dermis, with nodular distribution accompanied by thinning and fragmentation of the elastic fibers |
Once diagnosis is confirmed, it must be decided whether to extend the study and, if this is the case, the relevant additional tests must be selected. Several associations have been reported between familial connective tissue diseases and other diseases, principally affecting the heart.3 Shagreen plaques, for example, are a major criterion for establishing a diagnosis of tuberous sclerosis. One case of connective tissue nevus associated with macrodactyly and hemihypertrophy has been reported.8 However, to date, we have been unable to find evidence of diseases associated with zosteriform connective tissue nevus. Therefore, if neither the history nor a detailed physical examination reveals findings indicative of associated diseases, it is not necessary to continue with the study. Observation alone is sufficient.
As for clinical course, the lesions tend to be persistent and their prognosis depends on the presence of associated diseases. Treatment is only required in cases with major cosmetic repercussions.
In conclusion, we present a new case of a rare condition that fits the description of connective tissue nevus. The lesions had a peculiar, zosteriform-type distribution. Our case is unusual in that it involved 2 areas: the deltoid area and the lower back. We wish to stress the importance of ruling out familial cases because of their frequent association with other diseases, which would necessitate a more meticulous workup.
Please cite this article as: Castellanos-González M, Petiti-Martín G, Postigo C, Rodriguez-Peralto JL. Nevus de tejido conectivo con patrón zosteriforme. Aportación de un nuevo caso. Actas Dermosifiliogr.2012;103:640-642.