A 76-year old woman with no relevant past medical history visited our department with highly pruritic skin lesions that had appeared 6 years earlier. The patient did not associate the appearance of these lesions with any trigger factor. Additional tests requested, blood count, general biochemistry, hepatitis virus serology (HBV and HBC), HIV, syphilis, thyroid and autoimmune profile, chest x-ray, and tuberculin test (PPD) showed only abnormal levels of the following: glucose, 171 mg/dL; glycosylated hemoglobin, 8.33%; triglycerides, 386 mg/dL; and total cholesterol, 221 mg/dL.
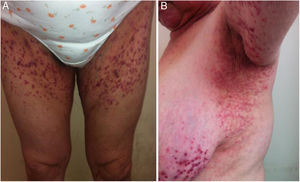
Physical ExaminationPhysical examination revealed a symmetric bilateral rash consisting of violaceous papules, some of which were even purplish, with a hyperkeratotic center, which coalesced in a retiform pattern, mainly on the flexor surface of the upper limbs (Fig. 1), the axillary folds, the root of the lower member and the groin, and on the torso (Fig. 2). The rest of the skin, nails and mucosa were not involved.
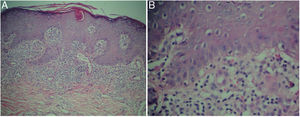
HistopathologyThe histologic study of a skin biopsy revealed irregular epidermal acanthosis with hyperkeratosis and follicular keratotic plugs, and a lymphocytic lichenoid inflammatory infiltrate in bands in the dermis, with foci of vacuolar damage in the basement layer of the epidermis, dilated blood vessels in the superficial plexus without vasculitis, and some extravasated red blood cells (Fig. 3). [[?]]What is your Diagnosis?
Chronic lichenoid keratosis.
Clinical Course and TreatmentTopical treatment was prescribed with a calcipotriol/betamethasone cream and oral prednisone at a dose of 1 mg/kg of weight; this achieved a considerable reduction in the pruritus and resolution of the papular lesions, leaving hyperpigmented postinflammatory patches, after 4 weeks of treatment.
CommentsChronic lichenoid keratosis or Nekam disease1 is a rarely reported and underdiagnosed entity.1–4 It was first described by Kaposi in 1895 as a variant of lichen, and dubbed lichen ruber acuminatus verrucosus et reticularis.1 In 1938, Nekam postulated that it was a variant of porokeratosis and therefore called it porokeratosis striata lichenoides. The current name of lichenoid keratosis was proposed by Margolis en 1972.1–4
It is a disease of unknown etiology, characterized by the presence of violaceous papules reminiscent of lichen planus, distributed over the torso and extremities in a linear and/or reticular symmetric, bilateral pattern, with a tendency to become generalized.4 Onset is usually in adulthood with no predominance of sex or race. It follows a chronic course, in which pruritus may vary from minimal or absent to very intense.1,4
It has been reported to coexist with facial lesions that simulate seborrheic eczema or perioral dermatosis, palmoplantar keratoderma, and dystrophic ungual lesions. In exceptional cases, the presence of oral or genital sores has been reported, and ocular lesions such as blepharitis, keratoconjunctivitis, or iridocyclitis.1,2
Histopathology is nonspecific. Focal parakeratotic hyperkeratosis is found with some follicular plugs. Vacuolization of the basement layer is present. A lymphocytic infiltrate in bands with a clearly defined lower limit can be seen in the upper dermis.2–5 A purplish variety has been described, characterized by hematic extravasation and occasional vasculitis.4 The differential diagnosis must include lichen planus, drug-induced lichenoid eruptions, pityriasis rubra pilaris, pityriasis lichenoides, mycosis fungoides, and other processes.2–5
The definitive diagnosis is established by means of a clinical-disease correlation where the main clinical sign is the retiform appearance of the dermatosis and the characteristic erythematous-violaceous coloring of the papules, in patients with no temporal association with medication. The histologic findings that support the diagnosis are lymphocytic lichenoid dermatitis with varying degrees of acanthosis, hyperkeratosis, and foci of parakeratosis. All these findings were present in the patient described. Treatment with daily application of calcipotriol/betamethasone cream was justified by the current understanding of the disease as a keratinization disorder,5,6 and the oral prednisone was justified by the intense pruritus, the considerable lymphocytic inflammatory infiltrate, and the extent of the lesions on the body. The patient’s diabetes was controlled with combination oral hypoglycemic agents, with no complications.
Conflicts of InterestThe author declares that he has no conflicts of interest.
Please cite this article as: Garzón Aldás E. Pápulas violáceas hiperqueratósicas confluentes retiformes. Actas Dermosifiliogr. 2020;111:601–602.