Defects of the anterior region of the pinna pose a reconstruction challenge owing to the complex topography and difficult access. We report our experience using the revolving door island flap (RDIF) to reconstruct pinna defects and present the surgical results.
Material and methodsRetrospective descriptive study of patients undergoing ear reconstruction using RDIF at different sites of the anterior region after resection of malignant tumors.
ResultsSeventeen patients underwent surgery between 2011 and 2019 for squamous cell carcinoma (n = 7) and basal cell carcinoma (n = 10). Conventional histology showed disease-free surgical margins in all the resected tissue specimens. The mean follow-up period was 40 months. One local recurrence of squamous cell carcinoma was observed, which responded well to radiation therapy; all patients were free of disease at the end of follow-up. Only 3 patients presented minor complications (depression of the flap surface in 1 case and retraction of the ear toward the mastoid process in 2 cases). Subjective rating scales were used to evaluate cosmetic and functional outcomes as assessed by both the dermatologist and the patient. The normal contour of the pinna was conserved in all patients and no patients required additional corrective surgery.
ConclusionsReconstruction of the pinna using RDIF allowed for satisfactory repair following complete resection of the tumors, while conserving structure and functionality. RDIF has been reported to be a very good option for reconstruction of the pinna. It is a simple technique that makes it possible to repair large defects with minimal risk of necrosis. In our series, the cosmetic results were excellent and recurrence rates were very low. RDIF provided optimal results in repairing lesions in the concha and in other regions, such as the antihelix, triangular fossa, and scapha.
Los defectos de la zona anterior del pabellón auricular (PA) son un desafío reconstructivo debido a la compleja topografía y el difícil acceso. Describimos nuestra experiencia con el uso del colgajo en isla en puerta giratoria (CIPG), para la reconstrucción de defectos auriculares y se presentan los resultados quirúrgicos.
Material y métodosEstudio descriptivo retrospectivo de pacientes sometidos a reconstrucción de oreja, de diversas localizaciones de la zona anterior, mediante el CIPG, tras la resección de tumores malignos.
ResultadosEntre 2011 y 2019 se operaron 17 pacientes: 7 carcinomas epidermoides y 10 basocelulares. El estudio histológico convencional mostró bordes quirúrgicos libres en todas las piezas de resección. El tiempo medio de seguimiento fue de 40 meses. Hubo una recidiva local en un carcinoma epidermoide, con buena respuesta a radioterapia, de forma que todos los pacientes estaban libres de enfermedad al completar el seguimiento. Sólo 3 pacientes presentaron complicaciones menores (depresión de la superficie del colgajo en un caso y retracción del oído hacia la mastoides en dos casos). Mediante escalas de valoración subjetiva, se determinó el resultado postoperatorio estético y funcional, tanto por parte del dermatólogo como del paciente. En todos los pacientes se conservó el contorno normal del PA reconstruido y ningún paciente requirió cirugía correctiva adicional.
ConclusionesLa reconstrucción auricular mediante CIPG permitió la reparación satisfactoria tras la resección completa de los tumores, preservando la estructura y funcionalidad. Está descrito que el CIPG es una muy buena opción reconstructiva de la concha auricular; es una técnica sencilla que permite reparar grandes defectos con mínimos riesgos de necrosis. En la serie presentada, el resultado cosmético fue excelente, con muy bajo índice de recurrencias. Los resultados son óptimos en la reparación de lesiones conchales pero también de otras zonas como el antihélix, las fosas triangular y escafoidea.
The pinna is a frequent site for cutaneous tumor development due to greater presence of actinic keratosis. Between 5% and 10% of nonmelanoma skin cancer (NMSC) develops in this area.1,2 Squamous cell carcinoma (SCC) at this site is associated with a higher rate of recurrence and greater metastatic potential. Likewise, basal cell carcinoma (BCC) of the ear can be histologically more aggressive than other head and neck sites and require more passes during Mohs surgery for complete excision.3 In general, the malignant tumors that develop on the concha of auricle have a higher risk of cartilage and inner ear involvement, increasing morbidity.4,5 Reconstruction of anterior ear defects is a therapeutic challenge due to the complex topography of the area, the reduced skin laxity, and difficult surgical access.1,2
Revolving door island flap (RDIF), also known as flip flop flap, postauricular island pedicle flap, pedicled retroauricular flap, is a subcutaneous pedicled pass-through flap harvested from the posterior or superior auricular area.2,6–9 It passes through the auricular cartilage to cover defects of the anterior pinna of the ear, and is used mainly for the concha of auricle.
Although the technique is considered a very good option for repair of anterior auricular defects arising from NMSC2,6 and from burns,10 few articles have been published on the final outcomes. It is an alternative to other techniques and yields good outcomes compared with healing by secondary intention or grafts.6,11 The technique is not widely accepted2,6 given its apparent complexity, although a randomized study showed that performing the procedure is simpler and faster than grafting.6 In Spain, surgeons expert in NMSC consider it as the technique of choice for lesions of the concha,12 although its versatility for reconstructing other areas, such as the antihelix or scaphoid fossa, is less well known.13
We present our experience and final outcomes with this flap procedure to reconstruct defects at different sites in the anterior area of the pinna after resection of malignant tumors.
Material and methodsThis was a descriptive, retrospective study of 17 patients with malignant tumors in the anterior pinna, reconstructed using RDIF over a period of 8 years between November 2011 and November 2019 in the dermatology department of the Hospital General Universitario, Ciudad Real, Spain. The medical history of the patients, tumor and surgical characteristics (duration of the tumor, site, size, resection margin, size of the surgical defect, and histopathological diagnosis) and events during follow-up (recurrence and short- and long-term postoperative complications) were reported. In addition, using subjective assessment scales (Tables 1 and 2), the esthetic and functional outcomes were assessed, both by the dermatologist and by the patients.2
Survey to Assess the Outcome of Surgery Administered to the Patient.
| [0,1–3]Scale of Patient Assessment | ||
|---|---|---|
| 5 | Very good (completely satisfactory) | The operated area appears completely normal. No differences can be noted compared with the other ear |
| 4 | Good (satisfactory) | The operated area has small imperfections, only obvious on close viewing (closer than normal distance in a conversation) |
| 3 | Regular (moderately satisfactory) | The operated area has moderate deformity, evident at a distance equal to or greater than a normal conversation |
| 2 | Poor (not very satisfactory) | The operated ear has completely lost its form. Further surgery is considered necessary to correct the defects |
| 1 | Very poor (not satisfactory) | There is functional impact (unable to wear glasses or headphones/hearing aids normally or impact on hearing) |
Modified from Iljin et al.5.
Scale to Assess the Esthetic and Functional Outcomes of Surgery Administered to the Dermatologist.
| [0,1–3]Scale of Dermatologist Assessment | ||
|---|---|---|
| 5 | Very good (completely satisfactory) | The reconstructed area has a contour, form, and color identical to the other ear |
| 4 | Good (satisfactory) | The reconstructed area has mild/evident imperfections at a distance of less than 1 m from the patient (flap depression, wound retraction, difference in pigmentation between surrounding tissue, or retraction of the ear towards the scalp) |
| 3 | Regular (moderately satisfactory) | The reconstructed area has moderate/evident imperfections at a distance of 1 m from the patientEsthetically pathological scarring at the donor site |
| 2 | Poor (not very satisfactory) | The operated ear has lost its normal architecture, but there is no functional impactScarring at the donor site is functionally pathological (contraction that impacts the mobility of the area) |
| 1 | Very poor (not satisfactory) | Functional impact (unable to wear glasses or headphones/hearing aids normally or severe constriction of the EAC)Additional surgical review necessary or referral to ear-nose-throat specialist |
Abbreviation: EAC, external auditory canal: Modified from Iljin et al.2;
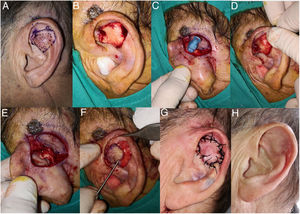
The procedure begins by marking the resection border of the tumor, ensuring a suitable surgical margin (4 mm for BCC, 4−6 mm for SCC) (Fig. 1A). Subsequently, depending on the site, the flap is designed in the retroauricular region. The flap will be rounded or oval-shaped, and the middle area should be centered on the retroauricular groove. The flap will therefore have skin harvested from the mastoid region and posterior face of the ear, while the central area, with the underlying pedicle included, will remain joined to the groove (Fig. 1D). Another technique to design the flap with a more precise size is to pass a needle through the borders of the surgical defect, from the anterior face towards the retroauricular area, and thus have reference points to define the borders of the flap (Fig. 1B and C) or simply make a template of the defect13 and center it on the retroauricular groove.
A, 80-year-old man with squamous cell carcinoma measuring 1.5 cm in the right concha of auricle. Delimitation of the resection margin. B and C, Design of the flap in the retroauricular area. To mark out the flap, a needle can be passed through the borders of the surgical defect from the anterior face to the retroauricular area. D, Flap design. The area corresponding to the subcutaneous pedicle should be centered on the retroauricular groove. E, Tumor excision. In addition, an area of auricular cartilage should be resected to make a slit for the flap to pass through to the anterior area. F, Flap dissected at its borders, attached in its central area to the groove. G, With forceps, the flap is passed through to the anterior part of the ear. H, Flap suture with 3/0 silk thread. I, Outcome 4 months after surgery.
Under local anesthetic with mepivacaine 2% or tumescent anesthesia, the tumor is excised with underlying cartilage if appropriate. In addition, a slit is opened in the auricular cartilage (Fig. 1E) to form a tunnel through which the flap will pass through to reach the anterior area. Then, the incision to form the flap is cut. The incision should be vertical towards the deep layers, towards the periosteum in the mastoid area and towards the perichondrium in the area of the pinna. This will enable a thicker and more mobile myocutaneous pedicled flap to be obtained. Once the flap has been released, we pass it through the slit in the cartilage to the anterior face of the ear using forceps (Fig. 1G). This movement is what gives the name to the technique: revolving door or flip flop.
The flap is attached to the anterior area with simple stitches with 3/0 or 4/0 nonabsorbable thread. The retroauricular area of the donor site is performed by direct closure.
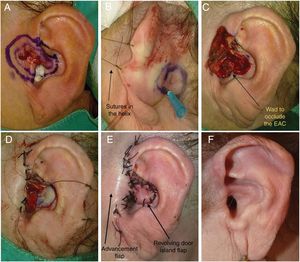
Before starting surgery, the external auditory canal should be blocked with a wad. For greater visibility of the retroauricular area, on making the incision for the flap, it is recommended to place a long suture in the helix to mobilize it and apply anterior traction to the pinna (Fig. 5B).
A good compressive bandage is useful and some authors recommend prophylactic antibiotic therapy to prevent chondritis,13 although the efficacy of such therapy has not been demonstrated.
ResultsA total of 17 flap procedures were performed (Table 3) in 13 men and 4 women. The mean age at the time of surgery was 78.1 years (range, 66–91 years). The tumors excised were 7 SCC and 10 BBC. There were tumors affecting more than one auricular region, with the most frequent sites being 8 cases in the auricle of concha (47%) and 8 in the antihelix (47%), followed by 3 in the triangular fossa (18%), and 1 in the scaphoid fossa (6%) (Figs. 2–5).
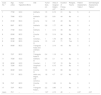
Epidemiological, Tumor, and Surgical Characteristics Scores on Scales to Assess Outcomes of Surgery.
| Case No.° | Age, y/Sex | Tumor Type(SCC/BCC) | Site | Tumor Size, cm | Area of Surgical Defect, cm2 | Duration of Follow-up, m | Relapse, Yes/no | Patient Assessment, Table 1 | Dermatologist Assessment, Table 2 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 77/M | SCC | Antihelix L | 1.5 | 6.15 | 31 | No | 5 | 4 |
| 2 | 79/M | SCC | Antihelix R | 2.5 | 9.61 | 44 | No | 4 | 3 |
| 3 | 81/M | BCC | Concha R | 1.2 | 3.8 | 43 | No | 5 | 4 |
| 4 | 89/F | BCC | Antihelix L | 0.8 | 1.77 | 40 | No | 5 | 4 |
| 5 | 77/M | SCC | Antihelix L | 1 | 3.14 | 39 | No | 5 | 4 |
| 6 | 83/M | BCC | Concha R | 1.5 | 3.14 | 38 | No | 5 | 5 |
| 7 | 66/M | BCC | Concha L | 1 | 1.76 | 26 | No | 5 | 5 |
| 8 | 91/M | BCC | Concha R | 1.5 | 4.9 | 71 | Yes | 5 | 4 |
| 9 | 84/M | BCC | Triangular fossa and antihelix R | 1 | 3.14 | 44 | No | 5 | 5 |
| 10 | 72/F | BCC | Triangular fossa R | 0.4 | 1.18 | 14 | No | 5 | 4 |
| 11 | 75/M | SCC | Antihelix R | 0.5 | 3.1 | 14 | No | 4 | 4 |
| 12 | 82/M | SCC | Concha L | 1 | 7.07 | 15 | No | 3 | 3 |
| 13 | 72/M | SCC | Scaphoid fossa | 2 | 6.15 | 61 | No | 4 | 3 |
| 14 | 80/M | SCC | Concha R | 1.5 | 4.9 | 88 | No | 5 | 4 |
| 15 | 77/F | BCC | Helix root, tragus, and concha L | 1.8 | 4.7 | 97 | No | 5 | 5 |
| 16 | 78/F | BCC | Concha R | 1.3 | 1.69 | 8 | No | 5 | 5 |
| 17 | 72/F | BCC | Triangular fossa L | 2.2 | 3.96 | 3 | No | 5 | 5 |
| mean | 78.1 | – | – | 1.27 | 4.13 | 40 | – | 4.67 | 4.07 |
Abbreviations: BCC, basal cell carcinoma; F, female; L, left; M, male; R, right; SCC, squamous cell carcinoma.
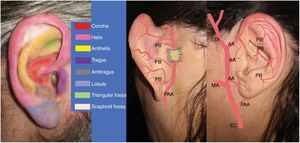
Schematic of the ear anatomy and the main anatomical areas. Arterial vascularization of the auricle of concha: posterior auricular artery (PAA) and its perforating branches (PB). External carotid (EC), maxillary artery (MA), anterior auricular arteries (AA), superficial temporal artery (STA).
A, 85-year-old man with basal cell carcinoma measuring 1.5 cm in the right superior concha and root of the helix. B, Design of RDIF. C, The flap incision should be deep and vertical towards the periosteum in the mastoid area and towards the perichondrium in the posterior face of the ear. D-F, The flap is made with a 90° rotation towards the anterior area, passing through the cartilage. G, Direct closure is performed in the defect in the root of the helix, whereas the flap is sutured in the concha. H, Outcome 2 months after surgery.
A, 72-year-old man with basal cell carcinoma measuring 1.8 cm in the root of the antihelix and left triangular and scaphoid fossae. B, Tumor excision sparing the underlying cartilage. C-E, Transfixion with needle in the resection margin marks the area to design the flap and resect cartilage. F and G, The flap is moved towards the anterior face of the ear and attached with simple stitches. The retroauricular area of the donor site is performed by direct closure. H, Outcome 1.5 months after surgery, maintaining structure and functionality.
A, 70-year-old woman with a complex basal cell carcinoma measuring 2.5 cm in diameter, affecting 4 areas (concha, root of the helix, tragus, and preauricular area). B, Design of RDIF. Placement of long sutures in the helix allows the auricle to be pulled forward to improve visualization of the surgical field. C, Resected tumor. D and E, The tragus, root of the helix, and preauricular areas are reconstructed with an advancement flap, whereas a revolving door island flap is used for the concha of auricle. F, Outcome 8 months after surgery. There had been no recurrences after 8 years of follow-up.
The tumor size varied between 0.5 and 2.5 cm (mean diameter, 1.27 cm). The surgical defect after excision ranged from 3.5 × 3.5 cm (9.61 cm2) to 1 × 1.5 cm (1.18 cm2), with a mean area of 4.13 cm2. The margin ranged from 4 to 10 mm, mean 5.4 mm, with a mean of 6.6 mm for SCC and 4.5 mm for BCC. Prophylactic oral antibiotics were administered after the procedure to prevent chondritis and wound infection in 2 patients who lived a long way from the clinic and who had difficulties attending the first dressing changes in the hospital.
The primary tumor resection piece included cartilage in 15 patients and only 2 had histological infiltration (1 BCC and 1 SCC), although this was partial and not full thickness. Conventional histological study showed disease-free borders in all 17 cases. Mohs surgery was only used in 1 patient with a recurrent tumor who had undergone prior resection in another center. The borders were disease-free after the first pass.
Regarding comorbidities in the patients, 82% (14 patients) had cardiovascular risk factors, 33.3% had dyslipidemia, 40% had diabetes mellitus, and 86.7% had hypertension. Four patients were receiving anticoagulation treatment (3 with acenocoumarol and 1 with rivaroxaban), which was suspended prior to surgery, and 4 were receiving antiplatelet agents (3 with acetylsalicylic acid and 1 with clopidogrel), which were maintained. Three patients had a history of malignant neoplasm (2 laryngeal carcinomas and 1 Hodgkin lymphoma) and 1 had received a kidney transplant.
The mean duration of follow-up was 40 months (range, 3–97 months). During this period, only 1 patient (5.8%) reported recurrence. This patient was a 91-year-old man, with BCC with cartilage involvement, who had undergone en-bloc resection with disease-free borders in the histological study. Recurrence was detected in the border close to the external auditory canal at 28 months after surgery. He was treated with radiotherapy, with good response, and is disease-free 6 years after surgery. Seven of the 17 patients (41%) died during follow-up, in all cases of causes unrelated to the tumor, and without any apparent recurrence at the time of death.
Three patients (18%) experienced minor complications; 1 patient developed depression of the flap surface and 2 experienced retraction of the operated ear towards the scalp or mastoid area. In one of these latter cases, the retraction reverted completely at 12 months. No patient presented flap bruising, infection, or necrosis.
To assess the esthetic and functional results, we applied subjective assessment scales,2 one administered to the dermatologist and the other to the patient during follow-up. The outcomes were assessed on a 5-point scale according to the characteristics of the physical examination and according to the degree of satisfaction in terms of cosmetic appearance (from very bad - 1 point - to very good - 5 points) (Tables 1 and 2). The postoperative assessments both by the dermatologist and by the patients are presented in Table 3. In both cases, the assessment was very positive. The normal contour of the reconstructed pinna was preserved in all patients and none of them required additional corrective surgery.
DiscussionReconstruction of skin defects in the anterior part of the ear, without altering its natural structure, is a surgical challenge.11,14 The main techniques used are flaps, grafts, and healing by secondary intention.11
Skin grafting is a valid and readily performed technique. It may be preferable from an oncological point of view, given the thin coverage would facilitate early detection of a possible recurrence. Drawbacks for this technique include a reduction in the structural firmness of the operated area. Furthermore, the centripetal constriction of the scar can affect the external auditory canal, and immobilization of the graft is more complex given the irregular contours of the ear, increasing the risk of subsequent hematoma and necrosis.6,15 The chances that the graft takes completely depends on preserving the perichondrium and partial removal of the cartilage.16 This technique may have worse esthetic outcomes depending on the texture and color of the skin, and because of the depression generated on the surface.2,5,11 It also takes longer to perform.6 One way to shorten these times is to use a split-thickness graft obtained from adjacent hairy skin.16 In the only comparative, prospective, randomized study, in 40 patients with skin cancer of the auricle of concha, cosmetic and functional outcomes were significantly better for the flap compared with grafting and the surgery time was shorter: 33 min (range 21–46 min) compared with 46 min for grafting (range 32–57 min). The authors concluded that the flap would be the technique of choice for defects of the concha.6
Healing by secondary intention is an option often used in this area,11,17 with very good cosmetic and functional outcomes. It is a very good option in small defects, or if we require a shorter surgery time in patients with several underlying conditions, although it would subsequently require a larger number of dressing changes.17 There is, however, a substantial risk of chondritis and infections and delay in wound healing can be noteworthy, particularly with larger defects.15,18
RDIF is a technique described in the literature for reconstruction of defects of the anterior face of the ear, mainly the auricle of concha, both due to tumor resection and burns.10 It was first described in 1972 by Masson and subsequently other authors have reported improvements in the original technique.7,19,20 It is characterized by harvesting skin from the ipsilateral retroauricular mastoid region. The anterior area of the pinna is irrigated by the superficial temporal artery that branches into 2–3 anterior auricular arteries while the retroauricular area is irrigated by the posterior auricular artery that includes perforating branches, such that both territories, anterior and posterior, are completely anastomosed. Furthermore, both arteries end forming a vascular arcade in the retroauricular groove to create a territory with extensive superficial and profound irrigation,11,21,22 formed of vessels from all directions, as demonstrated in cadavers.22 This makes it an excellent area for a pedicle relying on random vascularization as is the case for RDIF.14
The flap technique is simple and can be performed rapidly.11,14,23 It can be used to close large defects in a single surgical procedure (it has been described in the reconstruction of defects of up to 6 cm diameter24) with a minimal risk of necrosis.23 In a recent series, necrosis was reported in < 1% of cases (2 out 202 RDIF) and it was partial thickness.13 A larger diameter of the excised area requires a greater pedicle thickness and a wider tunnel, and this in turn favors the vitality of the flap and ensures appropriate surgical margins.7
Most authors recommend excising underlying cartilage when the tumor is resected.6,20 At least a partial resection of cartilage is needed, as this allows movement and the flap can be passed through from the retroauricular area to the anterior area.11 In fact, another name used for the procedure is a transcartilage island flap.13 At the time when the flap incision is made, care should be taken to ensure that this is deep and vertical towards the periosteum in the mastoid area and towards the perichondrium in the posterior face of the ear; this will help preserve irrigation from the retroauricular groove and improve the mobility of the flap.11 The donor site has lax skin, with identical color and texture to the anterior face of the ear, thus enabling the scar to blend with the surrounding skin.2,6,7 As a result, the cosmetic outcomes of the procedure are excellent.
As with all flaps, an appropriate surgical margin is crucial to ensure complete resection. Appropriate histological study of the piece is also essential. Mohs surgery is the technique of choice given the pinna is considered a site of risk. Most published series of RDIF did not use Mohs surgery5,6,9 and recurrences were not reported, although follow-up was short (mean of 24 months compared with 40 in our study). Indications for Mohs surgery have extended over time, and this technique is considered necessary for recurrent facial tumors as it has been shown to significantly reduce new recurrences at 5 years.25,26 Such recurrences are also common in primary BCC of more than 1 cm in areas of risk in the long term (10 years), 12% compared with less than 5% with Mohs surgery.27 Therefore, today, it is not recommended to perform RDIF in combination with conventional surgery without control of the margins. The risk is even greater for surgeons who are not expert in skin cancer and when there is suspicion of cartilage involvement. Faced with this suspicion, it is crucial to perform en-bloc cartilage resection for a good histological study of the piece and thus to ensure complete removal of the tumor. Cartilage is a good barrier and full-thickness involvement is rare; usually the tumor cords progress parallel to this anatomical structure. On resecting the cartilage to make a revolving door, if we leave borders with disease involvement, recurrence/persistence can spread towards the posterior plane leading to deep infiltration. It is therefore important to ensure disease-free borders when it comes to reconstruction with this technique. Marking the piece and detailed subsequent histological study is key. In a series of 17 cases and in more than 60 RDIF procedures published with cartilage resection without Mohs surgery, there was no recurrence at the base of the lesion.5,6,20
One of the disadvantages of this flap is that the retroauricular area is a surgical field that is difficult to visualize; this can be improved by placing sutures in the helix to pull the pinna forwards. Another disadvantage is the risk of retraction of the ear towards the scalp to create asymmetry with respect to the other ear,5,15,28 although it is hard to observe the 2 ears simultaneously. This effect is less notable in the concha, but in other concavities such as the antihelix or triangular fossa, the pinna may become too close to the mastoid region leading to a more visible asymmetry, particularly in those individuals without much hair.
The above notwithstanding, the cases presented in this series and those of other authors show that RDIF is a feasible solution not only in tumors of the concha, where it is the technique of choice,6,29 but also in antihelix defects, triangular fossa, and scaphoid fossa,13,14,20,23 with good outcomes.
In conclusion, reconstruction with RDIF enables complete resection of large tumors, conserving structure and functionality of the pinna, and with excellent esthetic outcomes. It is a procedure of medium difficulty that can be performed quickly (Table 4). Resection with sufficient surgical margin and good histological study, preferably with control of the margins, is crucial. RDIF is a good reconstructive option for the concha of auricle, and preferable to other techniques, especially when there is a lack of perichondria.5,7 The outcomes are just as good in other auricular areas such as the antihelix, suggesting that this flap is a versatile option for reconstruction of anterior defects of the ear, with a high success rate.
Tips for Successful Performance of Reconstruction by Revolving Door Island Flap (RDIF).
| Key for Performing RDIF |
|---|
| 1. Use generous surgical margins. This flap allows large defects to be reconstructed with minimal risk of necrosis (the larger diameter of the surgical defect implies a larger pedicle thickness) |
| 2. By using tumescent anesthesia with adrenaline minimizes pain in the infiltration, there is less bleeding and a longer duration of anesthetic. Use of adrenaline is not associated with auricular necrosis1 |
| 3. Resect cartilage underlying the lesion. This helps complete tumor resection and also facilitates movement of the flap |
| 4. Mohs surgery is the surgery of choice, and mandatory in recurrent tumors > 1 cm with aggressive histology. If this surgery is not possible, the piece should at least undergo detailed conventional histology study |
| 5. Center the pedicle of the flap on the retroauricular groove |
| 6. The flap incision should be deep and vertical down to the periosteum/perichondrium and then parallel to these structures, preserving vascularization of the retroauricular groove and increasing flap mobility |
| 7. The use of forceps can help pass the flap through to the anterior plane with the least possible trauma |
| 8. Occlude the external auditory canal during the whole procedure to avoid bleeding towards the eardrum |
The authors declare that they have no conflicts of interest.
Please cite this article as: Franco-Muñoz M, Romero-Aguilera G, Flores-Terry M, González Ruíz L, Rogel Vence M, Sánchez Caminero MP et al. Reconstrucción de defectos auriculares mediante el «colgajo en isla en puerta giratoria». Serie de casos. Actas Dermosifiliogr. 2020;111:590–599.