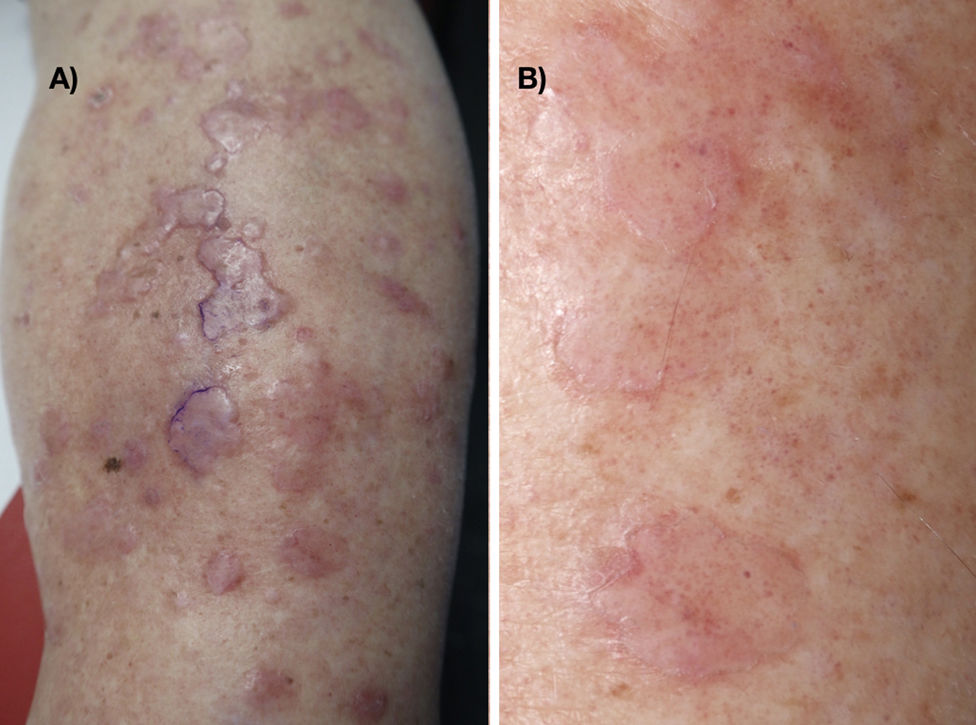
A 57-year-old obese woman with a history of disseminated superficial actinic porokeratosis (DSAP) involving the arms and legs, venous insufficiency, and secondary lymphedema presented with morphological changes in the DSAP lesions on the anterior aspect of both legs. She reported that the lesions had become increasingly palpable. Physical examination showed nonpitting edema in both lower limbs and well-defined flat erythematous-pink plaques with a scaling border alternating with other, more raised, plaques (Fig. 1A and B).
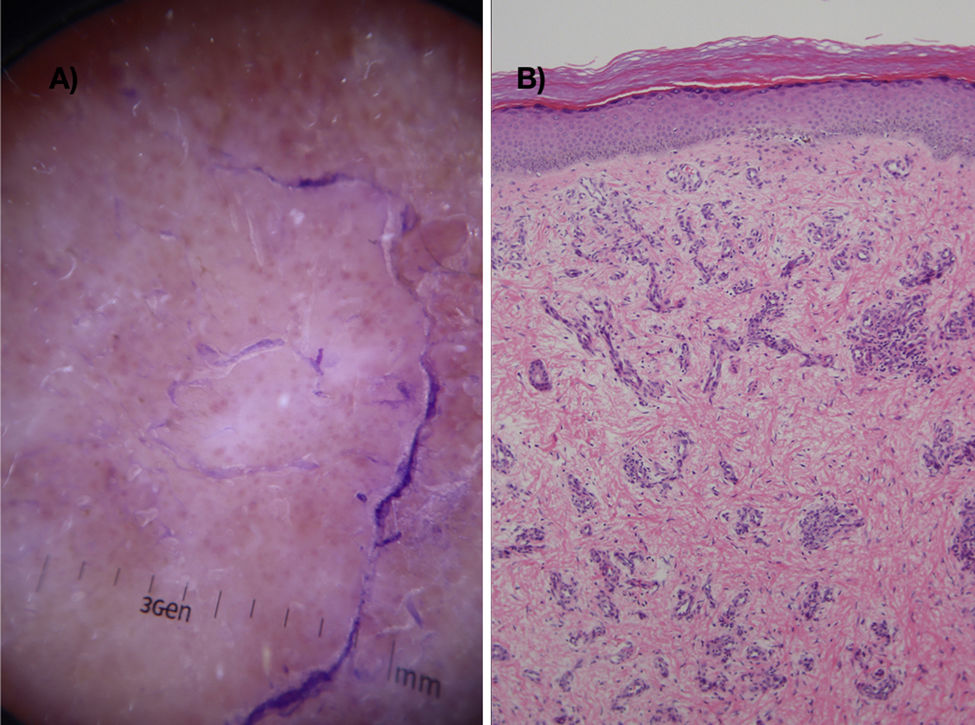
The furrow ink test highlighted the characteristic outlines of DSAP lesions (Fig. 1A and B). Dermoscopy of the lesions showed structureless white-pink areas with scales and dotted and glomerular vessels (red dots and globules) against a homogeneous background, visible inside and outside the raised lesions (Fig. 2A).
CommentPorokeratosis is a disorder of keratinization of unknown etiology. Seven clinical variants have been described: porokeratosis of Mibelli, DSAP, linear porokeratosis, punctate porokeratosis, porokeratosis palmaris et plantaris disseminata, porokeratosis ptychotropica, and eruptive disseminated porokeratosis. DSAP is characterized by flat papules and erythematous-brownish plaques with a well-defined hyperkeratotic border (the cornoid lamella on histology) and a slightly atrophic central area1. The clinical diagnosis is supported by observation of a peripheral white border, brown dots, a white central scar-like area, and dotted vessels on dermoscopy2. The furrow ink test is a useful adjunct for highlighting the cornoid lamella3.
Squamous cell carcinoma arising in porokeratosis lesions has been described in all clinical forms of this disorder except punctate porokeratosis1. The coexistence of porokeratosis and lymphedema, previously described in the literature, poses both a diagnostic and therapeutic challenge, as porokeratosis lesions, which are usually flat or mildly atrophic, can appear as raised plaques in patients with lymphedema, leading to possible confusion with neoplastic lesions4–6.
In the current case, in addition to characteristic clinical and dermoscopic features of porokeratosis, we observed multiple red globules, which at higher magnification appeared as glomerular vessels. Glomerular vessels in dermoscopy have been typically described in squamous carcinoma in situ, psoriasis, eczema, eccrine poroma, Merkel cell carcinoma, melanoma, Spitz nevus, actinic keratosis, and stasis dermatitis7.
The red globules inside and outside the DSAP lesions in our patient corresponded to dilated vessels in the papillary dermis (Fig. 2B). This dermoscopic and histologic pattern is consistent with stasis dermatitis.
Note should be taken of the increased risk of squamous cell carcinoma in this setting (due to the presence of both porokeratosis and chronic lymphedema), lymphangiosarcoma, Kaposi sarcoma, lymphoma, and melanoma arising from chronic lymphedema. It is important to biopsy fast-growing lesions, asymmetric hyperkeratotic lesions, and lesions with an atypical vascular pattern on dermoscopy.
In conclusion, dermoscopy is a useful tool for diagnosing stasis dermatitis and monitoring vascular patterns in lesions highly suspicious for malignancy, such as porokeratosis lesions in patients with venous insufficiency and lymphedema.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ramos-Rodríguez D, Del Pozo-Hernando LJ, Mestre-Bauzá F. Patrón vascular dermatoscópico en la poroqueratosis que coexiste con una insuficiencia venosa y linfedema. Actas Dermosifiliogr. 2021. https://doi.org/10.1016/j.ad.2019.12.011