A 5-year-old boy from Colombia with no known family history of skin disease presented with asymptomatic lesions on the limbs, predominantly in acral regions and areas around the joints. His family reported slow, peripheral growth of the lesions over the past few months but were unable to specify exactly when the clinical signs first appeared. No other associated symptoms were present at any level.
Physical ExaminationPhysical examination revealed keratotic, lichenoid plaques with mild peripheral erythema affecting the hips, acral regions, and areas around the joints on all 4 limbs, especially on extensor surfaces (Fig. 1). The development of the boy was normal for his age.
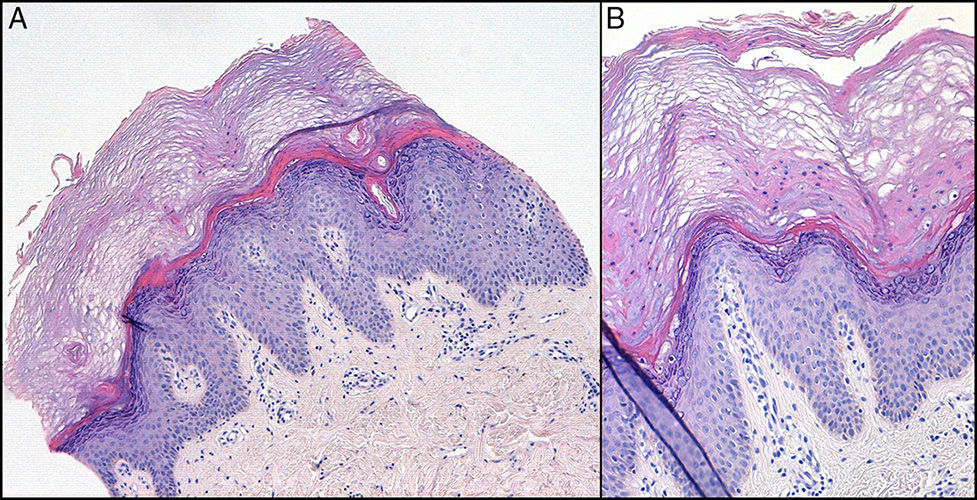
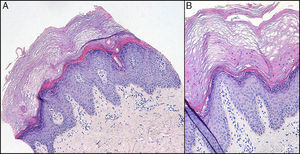
HistopathologyHistologic examination revealed hyperkeratosis with focal parakeratosis, hypergranulosis, and acanthosis with elongated rete ridges (Fig. 2).
What Is Your Diagnosis?
DiagnosisProgressive symmetric erythrokeratoderma (PSEK).
Clinical Course and TreatmentTopical treatment was started with 20% urea cream and systemic treatment was started with oral acitretin at a dose of 0.5mg/kg/d. Patient tolerance was good. Over several months, the lesions clearly involuted until they were limited to the acral regions of the limbs and the flexures, with a minimal effective dose of 0.3mg/kg/d. Periodic blood tests were carried out at follow-up visits, and no abnormalities caused by the treatment were observed. Adherence to treatment has been erratic over several years of follow-up at our dermatology clinic; periods of evident exacerbation have coincided with the voluntary withdrawal of the medication. The patient, now 14 years old, continues to receive treatment with acitretin at a minimum effective dose of 0.3mg/kg/d (Fig. 3).
CommentErythrokeratodermas are a clinically and genetically heterogeneous group of skin diseases characterized by well-defined erythematous-keratotic plaques.1–3 There are various subtypes, the most important of which are PSEK and erythrokeratoderma variabilis.4–6 PSEK is a rare genodermatosis that has been associated with a mutation in the loricrin gene on chromosome 1q21,1,4,5 although it is genetically heterogeneous.2 In most cases, PSEK is hereditary, with autosomal dominant inheritance, incomplete penetrance, and variable expressivity,1,2,6 although sporadic cases4,6 and cases with a recessive inheritance pattern2 have also been reported.
Clinically, PSEK is characterized by the appearance of large, erythematous, orange-colored, well-defined, symmetrical plaques that in some cases can have a keratotic or verrucous appearance, usually located on the buttocks, cheeks, and limbs.2,6 Palmoplantar involvement has been reported in up to 50% of cases.4,6 The lesions usually appear in the first years of life and spread slowly or remain stable during the following years; spontaneous improvement sometimes occurs, usually during puberty.1,6
Histologic findings are nonspecific, with foci of parakeratosis and marked acanthosis.1,4 Perinuclear vacuolization can be observed in the granular cell layer.4
PSEK is treated symptomatically. Topical treatments—including emollients and keratolytic agents—are reserved for the mildest cases.1,4 For severe cases, systemic treatment—oral retinoids, such as acitretin at a dose of 0.5mg/kg/d—is usually added. Psoralen-UV-A phototherapy has also been used, with variable clinical responses.1,4
We have presented a new case of PSEK, a rare entity. The case is unusual because it is sporadic, autosomal dominant inheritance being more common in this disease.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Santesteban Muruzábal R, Hervella Garcés M, Ros Martín C. ¿Qué genodermatosis es?. Actas Dermosifiliogr. 2014;106:667–668.