Hidradenitis suppurativa (HS) is a chronic inflammatory disease that arises in hair follicles in areas with a predominance of apocrine glands. It can cause major physical and psychosocial sequelae and its treatment is a significant challenge.1 Surgical elimination of the affected tissues is considered to be the treatment of choice.2 Severe axillary HS requires wide excision of the affected area, but reconstruction is complex and is associated with a high risk of postoperative complications. We used a pedicled parascapular flap in a patient with Hurley stage IIIHS.
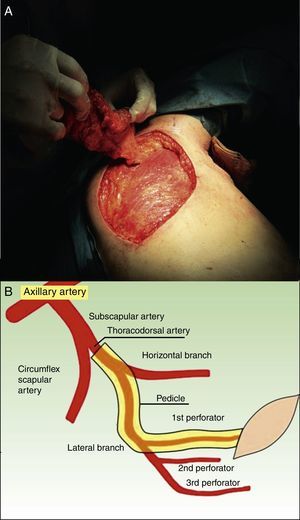
Description of the TechniqueThe thoracodorsal artery provides the main blood supply to latissimus dorsi. After giving off the branch to the serratus muscle, the artery bifurcates into a medial and a lateral branch. After an intramuscular path of 2cm, the lateral branch divides into 2 or 3 perforating arteries, the most proximal of which reaches the subcutaneous tissue 2 to 3cm posterior to the lateral margin of the latissimus dorsi muscle and 8cm inferior to the posterior axillary fold (Fig. 1B). The patient in placed in the lateral decubitus position with the arm abducted at 90° over the head. Ultrasound is used to locate and mark the thoracodorsal perforating artery in the superolateral region of the scapula, and the distance to the center of the homolateral axilla is measured; this will define the size of the flap. The flap is drawn and is carefully dissected until a pedicle is fashioned that includes the artery and permits sufficient mobility for the flap to be tunneled towards the axilla (Fig. 1A). All the affected area of the axilla is excised (Fig. 2A) and the tunnel to the scapular area is created. The flap is passed through the tunnel and is sutured by tissue planes. The defect left by the flap is also sutured by tissue planes (Fig. 2B). The immediate postoperative period is relatively short compared with a graft, and the patient can lead a normal life after the drain has been removed at 4 days. Two years after the operation in our patient there has been no recurrence, which he considers more than satisfactory (Fig. 2C and D). Furthermore, abduction has been fully preserved, as has also been reported by other authors.3
A, Appearance immediately after the en bloc excision of the affected axillary skin, with a surgical margin. B, Surgical wound after removal of the drain 4 days after the operation. C, Healthy axilla 2 years after the operation. D, Partial view of the donor site 2 years after the operation.
The pedicled parascapular flap has advantages over the use of grafts as recovery is much faster and the complication rate is much lower.2 However, operating time is longer (4hours) than for a graft (between 50 and 120minutes). Other surgical options to treat axillary hidradenitis include healing by second intention, which has the disadvantage of a long healing period and the tendency to provoke retractile scars in the area. Direct closure creates tension, which can lead to the progressive appearance of a dehiscent scar. Finally, a rotation flap from the adjacent skin can be a safe alternative, with a minimal risk of necrosis and little postoperative discomfort.
ComplicationsFlap necrosis is very unlikely if mobilization is performed carefully, with adequate dissection to avoid tension at the donor site where the artery arises. Torsion and compression of the flap pedicle must be avoided. If the artery is sectioned during the operation, the flap can be used as a graft.
ConclusionsWe have presented a method to treat severe axillary HS. Recovery is rapid and the cosmetic and functional results are magnificent, with a marked improvement in quality of life.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Eliseo Martínez García for the drawing in Figure 1B.
Please cite this article as: Tercedor-Sánchez J, Ródenas-López JM, Ramón-Faba P, Muñoz-Romero F. Colgajo paraescapular perforante para tratamiento de la hidradenitis axilar grave. Actas Dermosifiliogr. 2015;106:669–671.