Autosomal dominant skin diseases can sometimes present as linear mosaicism or as segmental mosaicism that follows the Blaschko lines. Type 1 mosaicism is characterized by the presence of a body segment affected by the disease in a healthy individual as a consequence of a postzygotic germline mutation in the segment. Type 2 mosaicism is characterized by the diffuse presentation of the disease in association with superimposition of a more involved body segment and is caused by the loss of heterozygosity in this segment during embryonic development in an individual who is heterozygous for the disease.1
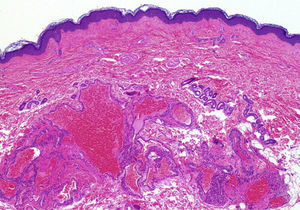
A 6-year-old girl with no personal history of interest presented with an asymptomatic segmentally distributed congenital bluish lesion that extended from the right groin along the medial aspect of the right thigh and leg to the right foot. The lesion had grown in proportion to the patient's own physical development. She also presented solitary nodular lesions that had begun to appear when she was 3 years old. These were painful to pressure and to changes in temperature and were scattered on all 4 limbs. Physical examination revealed a bluish plaque with palpable elastic nodules on the medial and posterior aspects of the right thigh and medial aspect of the right foot following a segmental course (Fig. 1). In addition, papules and nodules that were painful to pressure were observed on the contralateral foot and at distal sites on the other extremities. The patient's family history was remarkable in that her mother had scattered bluish nodular lesions (approximately 1cm in diameter) on the limbs and trunk that first began to appear during adolescence and were similar to those of the patient (Fig. 2). These lesions had not been examined previously. Biopsy specimens of the mother's lesions were taken, and histopathology revealed a new vascular formation in the deep dermis with wide vascular lumens filled with red cells and lined by glomus cells. The picture was consistent with glomuvenous malformations (Fig. 3). The congenital bluish plaque, the subsequent appearance of scattered lesions, and the mother's history of findings that were consistent with glomangiomatosis led us to make a diagnosis of type 2 mosaicism in familial glomangiomatosis. Given that the patient's quality of life is not affected, a wait-and-see approach with regular follow-up was adopted.
Glomangioma, or glomuvenous malformation, is a hamartoma of the dermal glomus bodies, which are responsible for temperature regulation. The 2 clinical forms described are solitary glomus tumor and glomuvenous malformations, or multiple glomangiomas. The first presentation is the more common and manifests typically in adults as painful isolated bluish nodules at acral sites. Glomuvenous malformations, or multiple glomangiomas, are characterized by the progressive early onset (infancy or adolescence) of scattered solitary bluish nodules or papules all over the body. Since the condition is autosomal dominant with incomplete penetrance or variable expressivity, a family history is only found in 60% of cases. This presentation has been shown to occur as a consequence of a mutation in the glomulin gene, which is present on chromosome 1p21-22.2 Congenital glomuvenous malformations are rare, and most cases of this manifestation reported to date are type 2 mosaicism, with an initial segmentally distributed lesion and subsequent appearance of distant scattered lesions, as in the present case. Familiar glomangiomatosis presenting as type 2 mosaicism was first reported by Happle and König.3 Our review of the literature revealed 9 subsequent cases with this clinical presentation2–9; therefore, 14 cases with this presentation have been reported to date, although none have been confirmed using molecular techniques. Besides being described in glomangiomatosis, type 2 mosaicism has been reported in several autosomal dominant diseases,10 although mosaicism has only been confirmed by genetic testing in a few of these cases.
In the case we present, it is clear that both the mother and the daughter present familial glomangiomatosis, even without confirmation by a genetic study. Given the clinical presentation as a superimposed congenital lesion in the daughter and the subsequent appearance of scattered lesions, we think that the present case can be considered a new example of type 2 mosaicism in glomangiomatosis.
Please cite this article as: de la Fuente S, Hernández-Martín A, Happle R, Torrelo A. Mosaicismo tipo 2 en glomangiomatosis familiar. Actas Dermosifiliogr. 2014;105:531–532.