Pemphigus herpetiformis (PH) is an uncommon variant of pemphigus that accounts for an estimated 6% to 7.2% of all cases of this skin disorder.1,2 The term pemphigus herpetiformis was coined by Jablonska et al.3 in 1975 to describe a entity that was clinically similar to dermatitis herpetiformis, showed acantholysis on biopsy, and responded to sulfapyridine. The authors considered that PH was a variant of pemphigus based on the direct immunofluorescence findings. PH typically presents with annular erythematous plaques, peripheral vesicles, and on occasions intense pruritus. Histologic features are highly variable and depend on the stage of the lesion. There have been reports of PH preceding or developing concurrently with pemphigus foliaceous (PF) or pemphigus vulgaris (PV).3–5 We present a case of PH that progressed to PF.
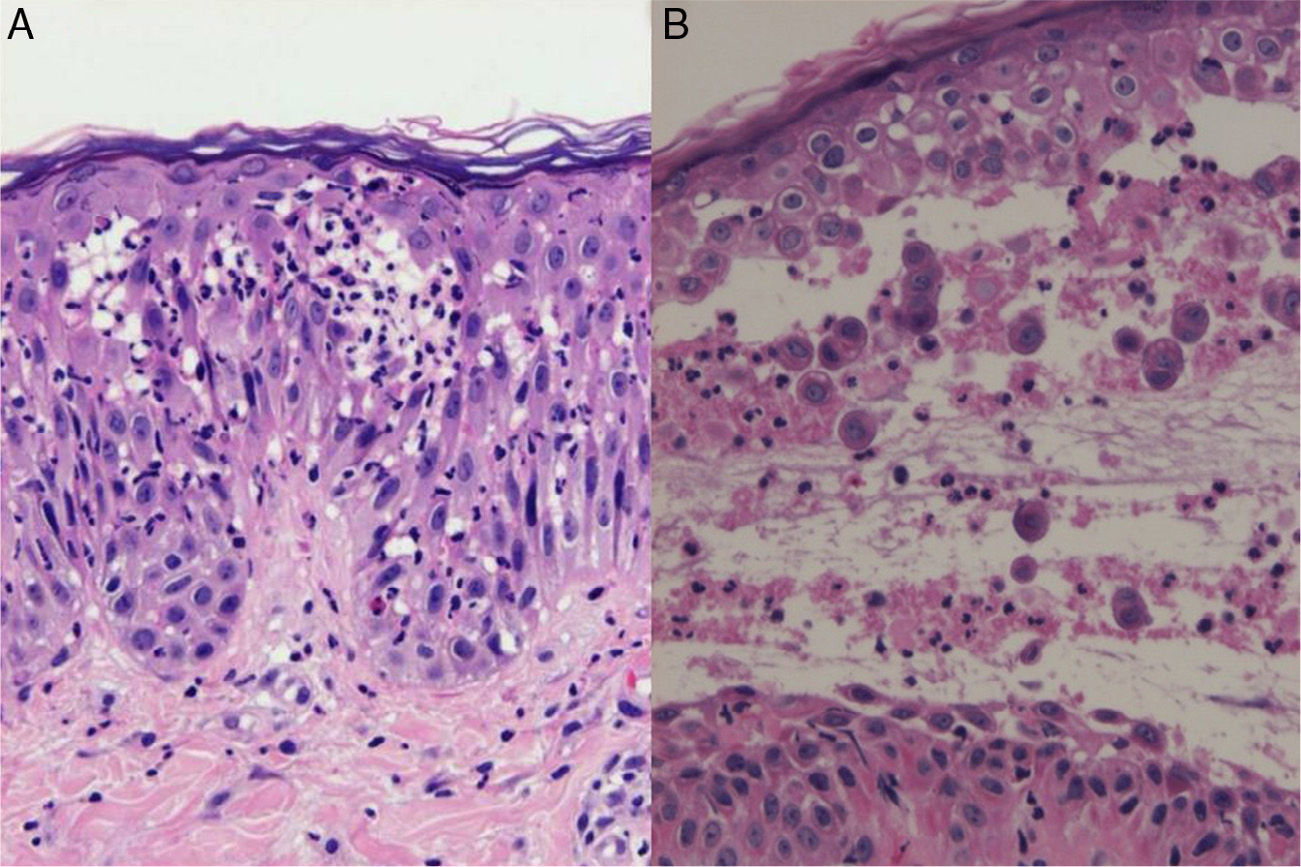
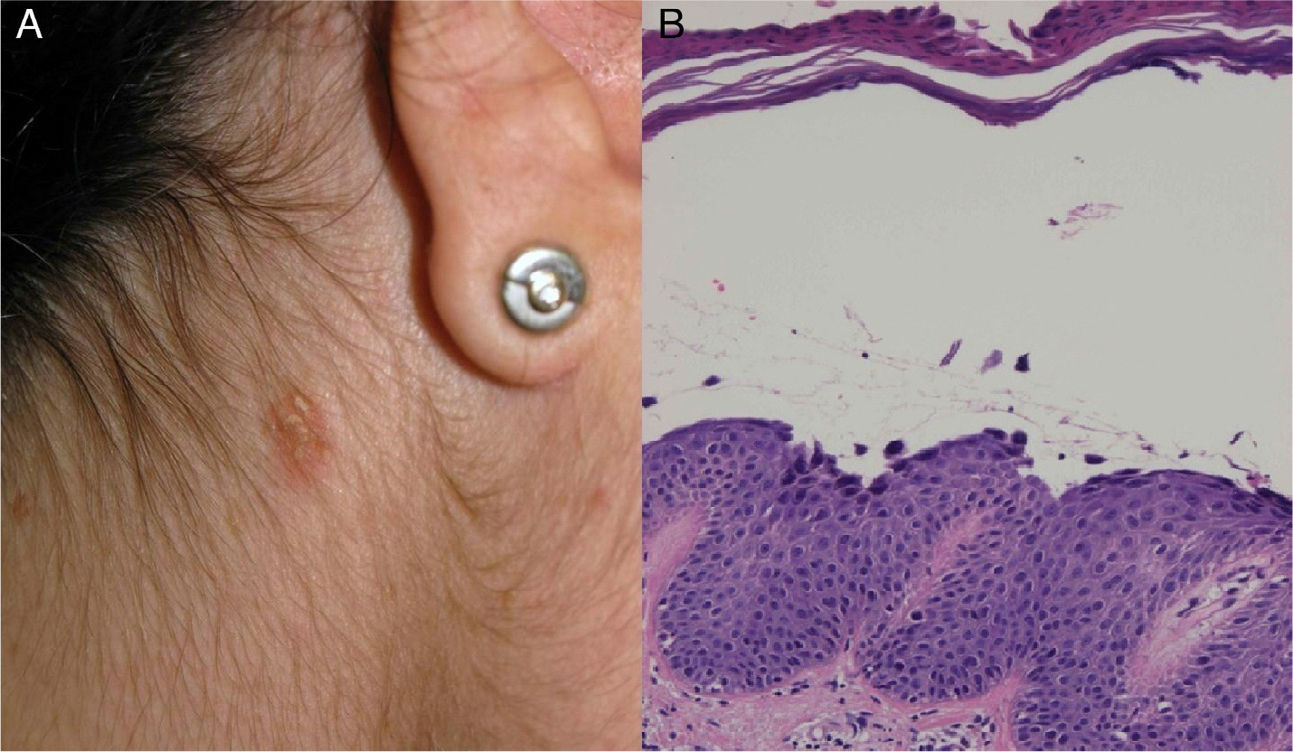
The patient, a 34-year-old woman with no relevant past history, consulted for erythematous papules and plaques with peripheral vesicles and blisters on the lower extremities, the abdomen, and the scalp (Fig. 1). The lesions had been present for 3 months. There was no mucosal involvement. Two biopsies revealed different degrees of neutrophilic and eosinophilic spongiosis (Fig. 2A) and acantholysis, with the formation of intraepidermal vesicles (Fig. 2B). Several eosinophils were also observed in the papillary dermis. Direct immunofluorescence showed intercellular immunoglobulin (Ig) G and C3 deposits, predominantly in the suprabasal layers of the epidermis. Anti-epithelial antibodies (titer, 1:40) and anti-desmoglein 1 (Dsg1) antibodies were positive (175 IU/mL; normal value, <20 IU/mL); the results for anti-Dsg1 antibodies were negative. A diagnosis of PH was made and treatment was started with prednisone 20mg/d and topical clobetasol. The lesions improved, but 3 months later, erythematous scaling plaques started to reappear in the presternal, dorsal, and retroauricular areas and on the scalp (Fig. 3A). Biopsy of one of these plaques showed a subcorneal acantholytic vesicle (Fig. 3B). The anti-epithelial antibody titer was 1:80 and anti-Dsg1 antibody levels remained high at 161IU/mL. Given the persistence of the lesions, treatment was started with dapsone 50mg/d, with dose increments up to 100mg/d. The clinical response was favorable and the dose was progressively reduced to 12.5mg every second day. Occasional flares consisting of minimal papules with scaling on the neckline, back, and scalp were observed.
PH is a variant of pemphigus that generally has a good prognosis, and most patients respond to sulfones.5 PH has a wide spectrum of clinical and histologic findings and accordingly numerous autoimmune blistering disorders must be considered in the differential diagnosis, namely, dermatitis herpetiformis, linear IgA bullous dermatosis, PF, PV, and bullous pemphigoid.6 Histologic findings can vary according to the stage of the disease and the type of lesion biopsied. Varying degrees of neutrophilic and/or eosinophilic spongiosis, with or without acantholysis in the middle and/or subcorneal layer, are observed. Kuhn et al.7 found that the inflammatory infiltrate in patients with PH was 68% eosinophil-dominant, 16% neutrophil-dominant, and 16% mixed eosinophil/neutrophil. We would like to stress the importance of performing direct immunofluorescence to test for the presence of an autoimmune blistering disorder when histology reveals neutrophilic and/or eosinophilic spongiosis.
Anti-Dsg1 and/or anti-Dsg3 antibodies have been described in most cases of pH,5,8 but there have been isolated reports of negative results for both antibodies.9
We have described an atypical course of PH that has been previously reported by Maciejowska et al.1 in 2 of 15 patients and by Santi et al.4 in 1 of 7 patients. There have also been reports of cases of PH developing after or at the same time as PF or PV.1,5 This possibility, together with the fact that anti-Dsg1 antibodies are detected in PH, has led to the hypothesis that PH and PF might be connected and that PH might actually be a variant of PF.4
It is not known why patients with PH, despite having anti-Dsg1 antibodies, have different clinical manifestations and histological findings to those with PF. Several hypotheses have been proposed. One is that in PH, IgG might cause keratinocytes to induce interleukin 8, whose chemotactic activity would explain the presence of a neutrophilic infiltrate.10 Another is that patients might develop antibodies that, despite their minimum acantholytic activity, could activate eosinophils and neutrophils through the Fc portion of IgG.5 Finally, it is possible that antibodies targeting epidermal antigens other than desmogleins or different epitopes might be responsible for the different phenotypic expression of pemphigus seen in PH.
Please cite this article as: Fuentes-Finkelstein P, Barnadas M, Gelpi C, Puig L. Pénfigo herpetiforme con evolución a pénfigo foliáceo. Descripción de un caso. Actas Dermosifiliogr. 2014;105:533–535.