Myiasis is a parasitic infestation of the tissues or organs of vertebrates (including humans) produced by the larvae of different species of fly (Diptera).1–3 It is classified according to the association between the parasite and the host and is described as obligatory, facultative, or accidental. It can also be classified according to the anatomic site of infestation as cutaneous, intestinal, or cavitary myiasis.1–3 Clinically, cutaneous myiasis is divided into furuncular, migratory, and wound forms.1–3 Incidence is higher in tropical countries with a humid climate and a low socioeconomic level.1–3
We present a case of autochthonous cutaneous myiasis caused by Chrysomya bezziana, a species that is exceptional in Europe.
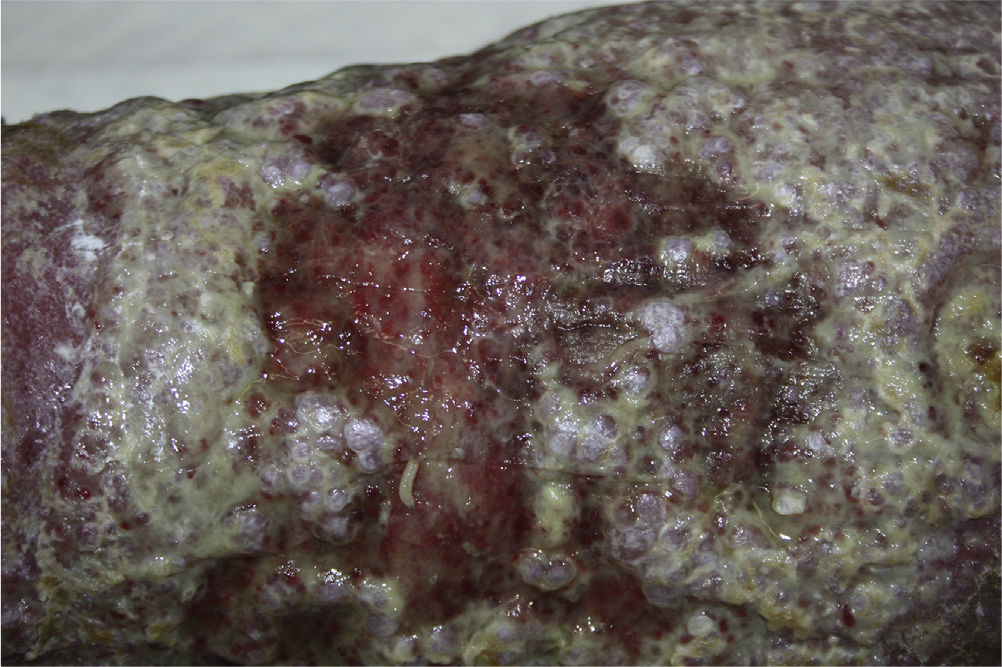
The patient was a 56-year-old man with a personal history of obesity, occasional alcohol consumption, arterial hypertension, sleep apnea-hypopnea syndrome, and extrinsic asthma. He was a heterozygous carrier of the PT20210A mutation, although he had no history of thrombosis. He had a vascular ulcer on the left leg that first appeared 10 months previously. Live larvae were detected during local care of the ulcer at his health center, from where he was referred to the emergency department. The patient had a good general status and denied having traveled abroad, recent contact with animals, or trips to the countryside. Physical examination revealed signs of chronic lymphedema in both legs. An ulcer was observed on his left calf. It measured 15×8cm, had an erythematous surface, and was papilliform in appearance. It was also friable, with malodorous exudate (Fig. 1). Several mobile Diptera larvae were identified on the lesion. These were whitish in color and in 1cm in length. They were eliminated mechanically and sent to the microbiology service for identification. The lesion was washed with saline solution and treated with an occlusive dressing of unscented pure petroleum jelly, and the patient was referred to the vascular surgery service. Macroscopically, the larvae extracted were identified as C bezziana; microscopically, subtle spine bands were visible around the body and the peritreme of the open posterior spiracle.
In developed countries, cutaneous wound myiasis is associated with poor hygiene, advanced age, psychiatric conditions, alcoholism, diabetes mellitus, and occlusive vascular disease.1–3
The 3 species that produce this form of myiasis throughout the world are Cochliomyia hominivorax (New World screw-worm), and C bezziana (Old World screw-worm)—both from the Calliphoridae family—and Wohlfahrtia magnifica, which belongs to the Sarcophagidae family.1–3 Most cases of autochthonous myiasis reported in Spain involve various species of the Sarcophagidae family (flesh fly).4
The parasite C bezziana is distributed in tropical and subtropical areas of Africa, southeast Asia, India, and the Middle East.1–4 It produces an obligatory form of myiasis that affects various domestic animals (cattle, horses, and pets) and, occasionally, humans.1,4 An adult female can deposit hundreds of eggs on the margin of wounds. The eggs hatch in 16hours, and the resultant numerous larvae feed for a week on the host's tissue. They then fall to the ground and complete their biological cycle to become adults.1,4 Under optimal conditions, the biological cycle lasts approximately 20 days.1,4 In humans, C bezziana produces wound infestations,4 skin tumors5, and cavities (orbit,6 mouth,7 and ear8), all of which have high morbidity. In severe cases, the patient can present with fever, a sensation of poor temperature regulation, pain, bacterial superinfection, leukocytosis with neutrophilia, or hypereosinophilia.2
In a review from the year 2000, the 47 species of Diptera responsible for myiasis in Spain did not include C bezziana.9 In the Spanish scientific literature, we found only 3 cases of human myiasis caused by this species: the first involved a 41-year-old Spanish man with a personal history of chronic alcoholism who developed cutaneous myiasis on chronic ulcers on the left leg that were secondary to rhabdomyolysis4; the second involved a 65-year-old Spanish woman with myiasis of the ear who reported no recent trips abroad8; and the third involved a 54-year-old Spanish man with myiasis on a supraglottic squamous cell carcinoma of the larynx that manifested as a tumor mass on the anterior aspect of the neck.6 International migration and climate change can explain, at least in part, why this species of fly is identified in countries that are not its natural habitat.10
In conclusion, we present a case of cutaneous myiasis on an ulcer in which C bezziana was identified as the causal agent. To our knowledge, this is the second case of autochthonous cutaneous myiasis caused by this species of fly. We wish to draw attention to this uncommon entity and to the importance of correct conservation and identification of larvae as part of routine clinical practice, since this condition is probably under-reported.
Please cite this article as: Aguado Lobo M, Hernández-Núñez A, Isabel García-Arata M, Borbujo J. Miasis cutánea no importada por Chrysomya bezziana. Actas Dermosifiliogr. 2014;105:529–530.