Vulvar lichen sclerosus et atrophicus (LEA) has a major impact on quality of life. Furthermore, it can degenerate into squamous cell carcinoma.1–3
Most patients can be managed with topical first- and second-line treatments. However, recalcitrant cases may require other forms of treatment, including retinoids, cyclosporine, or photodynamic therapy (PDT).3–5 These treatments are chronic and have limited efficacy; recurrence is frequent and adherence poor.2,4
Surgery is considered when structural alterations occur.6,7 CO2 laser has predominantly been used in cases of LEA of the penis. There are fewer reports of CO2 laser surgery in patients with vulvar LEA,4,7,8 and even fewer describing the use of fractional CO2 laser surgery.9 We have previously described treatment of extragenital LEA using fractionated erbium-yttrium-aluminum-garnet (Er:YAG) laser.10
We present 4 cases of biopsy-confirmed, long-standing vulvar LEA. The main clinical signs were itching, dyspareunia, and general discomfort with frequent appearance of wounds and erosions. All patients had received prior treatments that failed to provide effective control. One patient had undergone treatment with neodymium-doped:YAG (Nd:YAG) laser and another with cyclosporine and PDT (Table 1).
Presentation of the 4 Clinical Cases
| Case | Age, y | Diagnosis | Date of Onset (Clinical Signs) | Prior Treatments | No. of CO2 Laser Sessions | Response | Adverse Effects | Follow-up Duration, mo | Maintenance Regimen |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 60 | 2014 | Several years prior to diagnosis | Topical corticosteroid, lubricant | 7 | >75% | None | 16 | 2 sessions at 6 mo |
| 2 | 62 | 2015 | 1997 | Nd:YAG (2 sessions), oral ibuprofen, topical corticosteroid | 5 | >75% | Superficial ulcer | 5 | None |
| 3 | 53 | 2009 | 2006 (Effacement of the labia minora and narrowing of the introitus) | Topical corticosteroids and calcineurin inhibitors, EDF (antifungals + corticosteroids + Atb), topical anesthetic, oral metamizole, topical estrogens, oral cyclosporine, PDT, lubricants | 5 | >75% | None | 4 | None |
| 4 | 56 | 2017 | 2011 (Effacement of the labia minora and narrowing of the introitus) | Lubricants, topical corticosteroids | 5 | >75% | ACD (treated with EDF, anesthetic) | 10 | 1 session at 6 mo |
Abbreviations: Atb, antibiotic; ACD, allergic contact dermatitis: EDF, extemporaneous drug formulation; PDT, photodynamic therapy.
The patients were treated with a CO2 laser (Lumenis® AcuPulse) in deep fractional mode (15–17.5 mJ; density, 10–20%). Sessions were held at monthly intervals until achieving remission, which required a total 5 to 7 sessions per patient. Initially, CO2 laser treatment was performed under intralesional anesthesia. This was later replaced with topical anesthesia, which provided good pain control. Treatment was well tolerated and recovery time was fast. During this period, the use of topical antibiotics was advised. Antiviral prophylaxis was not administered as none of the patients had a history of genital herpes. Such prophylaxis would have been necessary in patients with a positive history. Patients did not undergo any concomitant treatment.
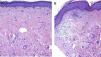
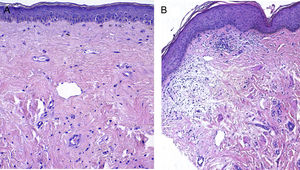
Treatment resulted in improvements in erythema, leukoderma, and skin elasticity, a reduction in erosions and fissures, and restoration of normal skin color and texture (Figs. 1 and 2). Histology revealed improvements in Patient 1 (Fig. 3). None of the other patients underwent post-treatment biopsy.
A, Pretreatment image showing epidermal atrophy, sclerotic collagen, and homogeneous hyalinization of the dermis (519.7 μm). B, Post-treatment image showing a more irregular, thicker epidermis, a thinner subepidermal hyaline band, and a loose dermis with greater cellularity and decreased hyalinization (376.5 μm).
All patients were very satisfied with treatment and rated their improvement as >75%. An improvement in clinical signs was evident after 1 to 3 sessions. Itching was the first sign to improve. Patient 1 experienced an increase in skin elasticity and an improvement in dyspareunia. This patient required more sessions, possibly due to the lower intensity of CO2 laser treatment in this particular case. Patient 2 reported a marked improvement in the burning sensation that previously limited her choice of clothing. This patient’s gynecologist also noted evident improvements. Moreover, the patient was able to resume sexual intercourse, which had previously been impossible. Patient 3 also attempted to resume sexual intercourse, which she had previously avoided due to fear of the resulting pain. That patient, who reported no improvements with any previous treatments, experienced evident improvements after the first session of CO2 laser therapy. Interestingly, a symptom diary maintained by this patient was left blank after the first few sessions. We consider these outcomes to be particularly significant, given that the patients had rated the impact of the disease on their quality of life at 8 or 9 on a 10-point scale. During follow-up, all patients remained free of clinical signs and required no further treatments. Three of the patients underwent subsequent intravaginal fractionated CO2 laser treatment to improve vaginal atrophy typical of menopause. Patients 1 and 4 underwent a single session of maintenance treatment after 6 months, in the former case due to persistent discomfort in the episiotomy area and in the latter due to the appearance of synechiae in a previously untreated area of the clitoris.
The effects of CO2 laser therapy are achieved by ablation of the epidermis by vaporization and by collagen remodeling caused by the residual thermal effect on the underlying dermis. This treatment modality offers some advantages over topical corticosteroids, including good adherence, and the absence of any local immunosuppression or atrophy. It provides effective, rapid results. It can induce collagen remodeling, reversing some of the damage caused. Furthermore, it could theoretically reduce the risk of malignant transformation as it is an effective ablative treatment for other premalignant lesions. Fractional CO2 laser allows rapid recovery, improves tolerance, reduces the risk of side effects, and can be performed in outpatient settings. We believe that it is a valid alternative for the treatment of uncomplicated, recalcitrant LEA and/or for maintenance therapy. Moreover, it could potentially be used for drug delivery, offering increased efficacy over conventional treatments. Disadvantages include the need for supporting infrastructure and the requirement of multiple treatment sessions when using fractional mode.
In conclusion, fractionated CO2 laser can be an effective and safe therapeutic alternative with a short recovery time for the treatment of vulvar LEA in certain patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We wish to thanks all patients who generously shared their experience for the purposes of this article in the spirit of helping other women.
Please cite this article as: Mendieta-Eckert M, Torrontegui Bilbao J, Zabalza Estévez I, Landa Gundin N. Tratamiento de liquen escleroso y atrófico vulvar con láser de dióxido de carbono fraccionado. Presentación de cuatro casos. Actas Dermosifiliogr. 2021;112:85–88.