To the Editor:
Most publications on the results of patch testing in patients with burning mouth syndrome (BMS) report high percentages of positive “clinically relevant” findings (between 13% and 74%), thus leading this approach to be considered a useful tool in the assessment of affected patients.1–3 Some authors point out that patients with intermittent symptoms (type 3 BMS) could be ideal candidates for patch testing.3 Various allergens are involved, and these are not always consistent from study to study, although most positive results are for metals, especially nickel.
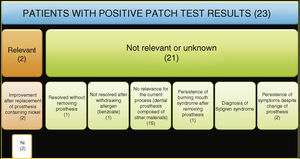
Taking the above into account, we performed a retrospective observational study in order to determine the clinical relevance of positive patch test results in patients with BMS. We analyzed the results of patch tests performed in patients diagnosed with BMS referred to our skin allergy unit over a period of 15 years (January 2001 to December 2015). We also followed patients via their electronic health records (Osabide Global) in order to determine the relevance of the positive results. During the period analyzed, a total of 2789 patients underwent testing. Of these, 67 had consulted for BMS (Fig. 1). The characteristics of the cohort were reported using the MOAHLFA index (Table 1). All patients with BMS underwent testing with the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea [GEIDAC]). Supplementary series were applied in 65 cases, depending on the clinical history. The most common were a dental series (Chemotechnique) (52.23%) and a metal series (Chemotechnique) (44.7%) (Table 2). Readings were made at 48 and at 96 hours following the recommendations of the European Society of Contact Dermatitis (ESCD). An allergic reaction was observed in 23 of the 67 patients (34.3%), with a total of 32 positive results recorded. Nickel was the main allergen (n = 11), followed by methylisothiazolinone/methylchloroisothiazolinone (n = 3) and beryllium (n = 3). We were able to establish present relevance in only 2 of the 67 patients with BMS (2.9%). In both cases, the patients were sensitized to the nickel in their dental prostheses; the symptoms resolved when the prostheses, which contained nickel, were removed. In the 21 remaining patients whose test results were positive, the results were considered to be not relevant or of unknown relevance for various reasons, mainly because of positive results to metals that were not a component of the dental prostheses they were wearing at the time (Fig. 1).
In the present study cohort, only 2.9% of the positive results were considered clinically relevant or with present relevance. This percentage is clearly lower than those reported in the literature.1–3 The cases considered as having present relevance corresponded to nickel, an allergen of the GEIDAC standard series. Therefore, the supplementary series used were not associated with an increase in the number of clinically relevant positive results diagnosed. Based on these findings, we believe that, except for selected cases where the clinical history points to an allergic origin for symptoms, patch testing should not be included in the routine evaluation of patients with BMS.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: De la Torre Gomar FJ, Heras González S, González Pérez R. ¿Suelen ser relevantes las pruebas epicutáneas en el paciente con síndrome de boca urente? Actas Dermosifiliogr. 2021;112:88–89.