Micrographic Mohs Surgery (MMS) offers the highest cure rates and healthy skin tissue sparing effect compared with standard excision.
ObjectiveTo quantify the tissue-sparing properties of MMS in squamous cell carcinoma (SCC) in comparaison with standard excision (SE).
MethodsA bidirectional, descriptive study, including 94 cases of SCC, was performed, on patients with histologic diagnosis of SCC (in situ, well differentiated, moderately differentiated, and undifferentiated), that where operated with MMS between 2013 and 2018 at Hospital de Clínicas “Dr. Manuel Quintela” in Montevideo, Uruguay. Tumor size and defect area after MMS were measured in 2 perpendicular directions. The suspected defect area was calculated with standard excision using a 4-mm margin for low risk lesions and a 10-mm margin for high risk lesions. The primary outcome of this study was the size of the defect area post MMS compared with the calculated defect area with standard excision.
ResultsThe median tumor size was 1,41 mm2, and the median defect size after MMS was 4,12 mm2. The median defect size calculated for standard surgical excision was 8,36 mm2.
LimitationsWe do not use all National Comprehensive Cancer Network (NCCN) criteria. We define low and high risk lesions just taking into account anatomical location, size, histopathology and whether it was a primary or recurrent tumor.
ConclusionOur results show that MMS has a tissue-sparing effect of at least 52% compared to SE.
La cirugía micrográfica de Mohs (CMM) es la técnica que ofrece las tasas más altas de curación, así como la mayor capacidad de ahorro de tejido sano, en comparación con la extirpación estándar.
ObjetivoCuantificar la capacidad de ahorro del tejido de la CMM en el carcinoma de células escamosas (CCE) en comparación con la extirpación estándar (EE).
Material y métodosSe realizó un estudio de tipo descriptivo bidireccional, para el cual se incluyeron un total de 94 casos de CCE. Los pacientes habían sido diagnosticados de un CCE (in situ, bien diferenciado, moderadamente diferenciado e indiferenciado) e intervenidos mediante CMM en el Hospital de Clínicas Dr. Manuel Quintela, en Montevideo, Uruguay, entre los años 2013 y 2018. Tanto el tama˜no del tumor como el área resultante del defecto tras la CMM se midieron tomando las dos medidas del tumor perpendiculares entre sí. El área hipotética calculada del defecto tras la extirpación estándar se estimó agregando un margen de seguridad de 4 mm enlas lesiones de bajo riesgo y de 10 mm en las lesiones de riesgo elevado. El resultado primario de este estudio fue determinar el tama˜no del área del defecto tras la CMM en comparación con el área del defecto calculado si el tumor hubiera sido intervenido mediante una extirpación estándar.
ResultadosEl tamaño medio del tumor fue de 1,41 mm2 y el tamaño medio del defecto tras la CMM fue de 4,12 mm2. El tamaño medio del defecto calculado para la extirpación quirúrgica estándar fue de 8,36 mm2.
LimitacionesNo se utilizaron todos los criterios de la National Comprehensive Cancer Network (NCCN). Las lesiones de riesgo bajo y elevado se definieron teniendo en cuenta la ubicación anatómica de la lesión, el tamaño, la histopatología y si se trataba de un tumor primario o de una recidiva.
ConclusiónLos resultados del presente estudio demostró un ahorro de al menos el 52% con la CMM en comparación con la EE.
Squamous cell carcinoma (SCC) is the second most common skin cancer. Some studies show that SCC incidence rates are rising more rapidly than the rates of basal cell carcinoma (BCC).1
Mohs micrographic surgery (MMS) is a technique for the excision of skin cancer, especially SCC and BCC. The main advantage of MMS over standard excision is the possibility of complete tumor removal through histologic examination of a 100% of the surgical margin, achieving superior cure rates.2,3 Another benefit described for MMS is healthy skin tissue sparing. Conservation of healthy tissue is a matter of interest especially when it affects areas such as the face. Numerous studies have proven the efficacy and safety of MMS, but there is little information of the amount of tissue spared with this technique, specially in SCC.
The aim of this study was to determine the amount of tissue spared with MMS compared with standard excision (SE).
PATIENTS AND METHODSWe inclued all patients with a histologically verified SCC who underwent MMS from November 2013 to November 2018 in the Dermatologic Surgery Unit at Hospital de Clínicas “Dr. Manuel Quintela” in Montevideo, Uruguay.
Data obtained from surgical clinical history, epidemiological and clinical information (sex, age and phototype), tumor characteristics (anatomical location, size, histopathology, primary or recurrent, and risk level accordingly), as well as the defect size, were determined. All patients underwent MMS for presenting at least one high risk criteria of the NCCN. For our study we define low risk lesions as those located in amedium-risk area with tumor size smaller than 10 mm, or low-risk area smaller than 20 mm and if the histopathological result was: well differentiated, without perineural involvement and thickness less than 2 mm. High-risk tumors were define as those located in a high-risk area, medium-risk area and greater than 10 mm or in low-risk area greater than 20 mm, if is was a recurrence and if the histopathological result was poorly differentiated, acantholytic, adenosquamous or desmoplasic subtype, perineural involvement and thickness more than 2 mm.4
Tumor and defect areas were estimated based on their usual round to oval shape, with the formula: 0,25 × π × longest radius × perpendicular radius to the longest one. Digital photographs were taken. The area of the defect for the hypothetical SE was calculated using the mentioned formula adding 4 millimeters in each radius for the low risk tumors and 10 millimeters in each radius for the high risk ones.5,6
The study was approved by Ethics Committee of "Hospital de Clínicas Dr. Manuel Quintela", University of the Republic.
STATICAL ANALYSISThe variables were register in a MsExcel® spreadsheet. STATA 11.0® was used for statistical analysis.
RESULTSWe included 72 patients (43 men, 29 women) with 94 SCC. The mean age was 75 years (range: 30-92 years). According to the phototypes of Fitzpatrick, 2 patients were phototype I, 29 patients were phototype II, 39 patients photoype III and 2 patients phototype IV.
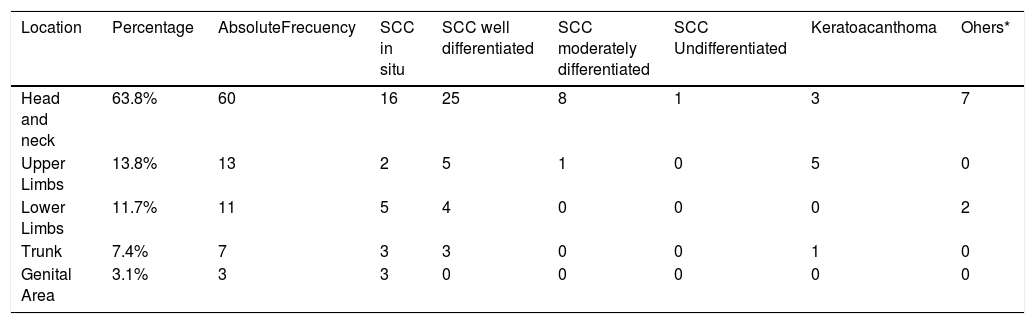
The number of tumors, locations and histopathological subtype are shown in Table 1. 60 Lesions (63,8%) were located in the head and neck, 19 in cheeks, 12 in the auricular and periauricular areas, 6 in lips, 5 in nose, 5 in the periocular area, 5 in the scalp, 4 in the forehead, 3 in the temple and 1 in the perioral area.
Topography and histological variant of the lesions.
| Location | Percentage | AbsoluteFrecuency | SCC in situ | SCC well differentiated | SCC moderately differentiated | SCC Undifferentiated | Keratoacanthoma | Ohers* |
|---|---|---|---|---|---|---|---|---|
| Head and neck | 63.8% | 60 | 16 | 25 | 8 | 1 | 3 | 7 |
| Upper Limbs | 13.8% | 13 | 2 | 5 | 1 | 0 | 5 | 0 |
| Lower Limbs | 11.7% | 11 | 5 | 4 | 0 | 0 | 0 | 2 |
| Trunk | 7.4% | 7 | 3 | 3 | 0 | 0 | 1 | 0 |
| Genital Area | 3.1% | 3 | 3 | 0 | 0 | 0 | 0 | 0 |
There were 80 (85,1%) primary tumors and 14 (14,8%) relapsing lesions. Of the last group, 5 relapses after standard tumor excision, 2 after MMS and 7 after other treatments (cryosurgery, imiquimod or cryosurgery + imiquimod).
Considering tumor size, anatomic localisation and whether if it was a primary or relapsing tumor, 77 (81,9%) lesions were catalogued as high risk lesions, and 17 (18,08%) as low risk ones. Of all lesions, 47 (50%) were in high risk zones and 24 (25,5%) in low risk zones.
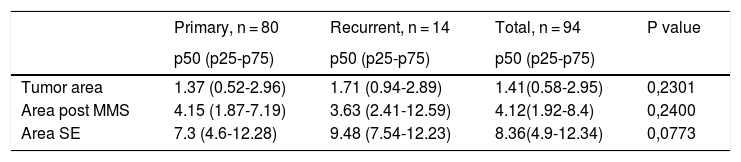
Regarding primary and recurrent tumors, as shown in Table 2, there were no statistically significant differences between the area of the tumor, the defect area post MMS and the calculated defect area.
Median of diferents varibles for low and high risk tumors. Micrographic mohs surgery (MMS). Standard excision (SE). Mann-Whitney test.
| Primary, n = 80 | Recurrent, n = 14 | Total, n = 94 | P value | |
|---|---|---|---|---|
| p50 (p25-p75) | p50 (p25-p75) | p50 (p25-p75) | ||
| Tumor area | 1.37 (0.52-2.96) | 1.71 (0.94-2.89) | 1.41(0.58-2.95) | 0,2301 |
| Area post MMS | 4.15 (1.87-7.19) | 3.63 (2.41-12.59) | 4.12(1.92-8.4) | 0,2400 |
| Area SE | 7.3 (4.6-12.28) | 9.48 (7.54-12.23) | 8.36(4.9-12.34) | 0,0773 |
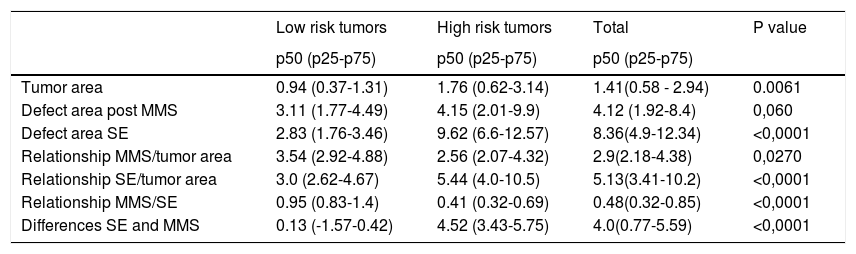
The median tumor surface area for low risk tumors was 0.94 cm2, the median defect area post MMS was 3.11 cm2 and the median defect area calculated for SE was 2.83 cm2. The median tumor surface area for high risk lesions was 1.76 cm2, the median defect area post MMS was 4.15 cm2 and the median defect area calculated for SE was 9.62 cm2.
Taking into account the relationship between the area of the tumor and the defect area of MMS, the median was 3.54 cm2 for low and 2.56 cm2 for high risk lesions respectively. Regarding the relationship between the area of the tumor and the defect area calculated for SE, the median was 3.0 cm2 for low, and 5.44 cm2 for high risk lesions.
We found a statistically significant difference between the post MMS defect area and the calculated defect area for SE. The median was 0,95 for low risk lesions and 0.41 for high risk lesions. The diference between the defect area calculated for SE and Mohs 4.52 cm2 for high and 0.13 cm2 low risk lesions respectively.
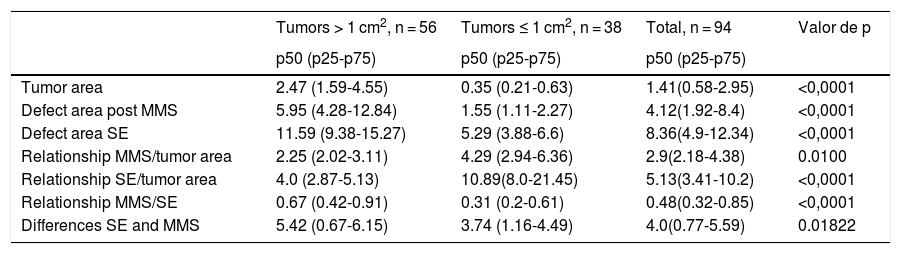
56 SCC were catalogued as tumors larger than 1 cm2 and 38 SCC as tumors smaller than 1 cm2. The relationship between them is are shown in Table 4.
DISCUSSIONFew studies have quantified the tissue-sparing properties of MMS compared with SE, all of them focusing in basal cell carcinomas.
The tumor area and the area of the defect, for both MMS and SE, was significantly greater in high-risk lesions. For low risk lesions, the final defect was 3,54-fold the size of the tumour after MMS and the defect area calculated for SE was 3 times the tumor lesion. As outlined in Table 3, in at least 25% of these tumors, SE with a 4-mm margin would have led to inadequate tumor removal.
Median of diferents varibles for low and high risk tumors. Micrographic mohs surgery (MMS). Standard excision (SE). Mann-Whitney test.
| Low risk tumors | High risk tumors | Total | P value | |
|---|---|---|---|---|
| p50 (p25-p75) | p50 (p25-p75) | p50 (p25-p75) | ||
| Tumor area | 0.94 (0.37-1.31) | 1.76 (0.62-3.14) | 1.41(0.58 - 2.94) | 0.0061 |
| Defect area post MMS | 3.11 (1.77-4.49) | 4.15 (2.01-9.9) | 4.12 (1.92-8.4) | 0,060 |
| Defect area SE | 2.83 (1.76-3.46) | 9.62 (6.6-12.57) | 8.36(4.9-12.34) | <0,0001 |
| Relationship MMS/tumor area | 3.54 (2.92-4.88) | 2.56 (2.07-4.32) | 2.9(2.18-4.38) | 0,0270 |
| Relationship SE/tumor area | 3.0 (2.62-4.67) | 5.44 (4.0-10.5) | 5.13(3.41-10.2) | <0,0001 |
| Relationship MMS/SE | 0.95 (0.83-1.4) | 0.41 (0.32-0.69) | 0.48(0.32-0.85) | <0,0001 |
| Differences SE and MMS | 0.13 (-1.57-0.42) | 4.52 (3.43-5.75) | 4.0(0.77-5.59) | <0,0001 |
Median of diferents varibles for tumors ≤1 cm2 and >1 cm2. Micrographic mohs surgery (MMS). Standard excision (SE). Mann-Whitney test.
| Tumors > 1 cm2, n = 56 | Tumors ≤ 1 cm2, n = 38 | Total, n = 94 | Valor de p | |
|---|---|---|---|---|
| p50 (p25-p75) | p50 (p25-p75) | p50 (p25-p75) | ||
| Tumor area | 2.47 (1.59-4.55) | 0.35 (0.21-0.63) | 1.41(0.58-2.95) | <0,0001 |
| Defect area post MMS | 5.95 (4.28-12.84) | 1.55 (1.11-2.27) | 4.12(1.92-8.4) | <0,0001 |
| Defect area SE | 11.59 (9.38-15.27) | 5.29 (3.88-6.6) | 8.36(4.9-12.34) | <0,0001 |
| Relationship MMS/tumor area | 2.25 (2.02-3.11) | 4.29 (2.94-6.36) | 2.9(2.18-4.38) | 0.0100 |
| Relationship SE/tumor area | 4.0 (2.87-5.13) | 10.89(8.0-21.45) | 5.13(3.41-10.2) | <0,0001 |
| Relationship MMS/SE | 0.67 (0.42-0.91) | 0.31 (0.2-0.61) | 0.48(0.32-0.85) | <0,0001 |
| Differences SE and MMS | 5.42 (0.67-6.15) | 3.74 (1.16-4.49) | 4.0(0.77-5.59) | 0.01822 |
In high risk lesions, the defect area calculated for SE double the defect area post MMS, 5,44 and 2,56 fold tumor area, respectively.
In 11 of the 94 tumors (11.7%), the calculated defect size in SE was smaller than the Mohs defect size, resulting in inadequate tumor removal. Three of them were high risk tumors.
The relationship between the MMS defect area and calculated SE defect area of show that there was not much tissue sparing with MMS in low risk SCC. MMS was tissue-sparing compared with a SE with pre-determined margins for high risk lesions by 59%. However, regardless of the risk level of this lesions, our studies show 52% tissue sparing effect with MMS.
Our study shows that there were statistically significant differences between defect area post MMS and calculated defect area for SE in tumors smaller than 1 cm2 as well as larger than 1 cm2.
To our knowledge, this is the first bidirectional descriptive study that quantifies the MMS tissue sparing properties in SCC. Gniadecki and col.7 performed a retrospective study of 263 cases of basal cell carcinoma (BCC), where 54% of them were primary tumors. Their results show that the area of the excision can be reduced by > 40% by using the micrographic technique rather than SE with predetermined margins.
A study conducted by Muller and col.8 included 30 tumors with clinical diagnosis of a nodular BCC less than 1 cm in diameter. High risk lesions were excluded. Patients were randomly assigned to either MMS or standard surgery. The median area of the surgical defects in the MMS group was 116.6 mm2, versus 187.7 mm2 in the standard surgery group with 4 mm margin (95% CI = 61–126, p < .001), that is, a median with standard surgery 1.6 times the area with MMS.
A recent prospective study performed by Van Kester and col.9 with the which objective of quantifying the tissue-sparing properties of MMS in primary BCC with an infiltrative growth pattern include 256 lesions. The suspected defect surface area with standard excision was calculated using a 5-mm margin. They show that MMS had a 46.4% tissue-sparing effect when compared with standard surgical excision (95% confidence interval, 43.4%-49.1%; P value<.001).
CONCLUSIONSMMS had tissue-sparing effect by 52% in SCC. The tissue-sparing effect was higher for high risk tumors. MMS removed less healthy skin tissue compared with SE, 33% tissue sparing effect in lesions >1 cm2 and 69% in tumors <1 cm2.
FundingNone.
Conflict of InterestDr. Julio Correa is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. All authors declare having no conflicts of interests of any kind.
Please cite this article as: Correa J, Pastor M, Céspedes E, Magliano J, Bazzano C. Ahorro de tejido tras la cirugía micrográfica de Mohs en los carcinomas de células escamosas. Actas Dermosifiliogr. 2020;111:847–851.