The treatment of choice for lentigo maligna (LM) and for lentigo maligna melanoma (LMM) is still complete excision of the tumor with adequate surgical margins. Conventionally, surgical margins of 0.5cm for LM and of 1cm for thin LMM with a Breslow depth<1mm have been recommended. However, numerous reports have demonstrated the need for wider margins, as the subclinical extension of the melanocytic dysplasia in LM can be greater than predicted.1-4 Techniques with 3-dimensional histological control of the margins have been found to be better than conventional surgery as they are followed by fewer recurrences.4,5 Since 2008, the National Comprehensive Cancer Network recommends the use of these techniques whenever possible.
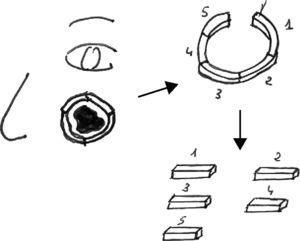
Our first patient was an 84-year-old woman who presented an irregularly pigmented lesion of 2.5cm that had been present for 4 years on her left cheek; biopsy confirmed LM. The so-called spaghetti technique (initial delimitation of the perimeter of the lesion) (Fig. 1) was chosen. This technique consists of the excision of a strip of tissue with a breadth of about 3mm around the perimeter of the lesion; the wound is then sutured and the patient can go home with a closed wound to await the histology report (Fig. 2). The specimen is fixed in formol by sectors and marked so that the pathologist can process it as usual and take vertical sections after embedding the tissue in paraffin. If necessary, based on findings, the surgical margins can be enlarged until free margins are achieved. Complete excision of the lesion is then performed, with closure of the defect using a flap if indicated. In this patient, free margins were achieved with excision of the first strip of tissue and complete excision of the lesion could be performed the following week.
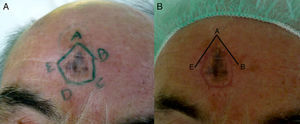
Our second patient was a 69-year-old man with a 2-cm LM on the forehead. In this case, a polygonal excision was designed to match the outline of the lesion and the skinfolds of the forehead (Fig. 3). It was necessary to extend the margin in the superior zone in a second operation (Fig. 3B). Complete excision of the lesion and closure of the defect was performed 20 days after the first operation.
The spaghetti technique is not new, but rather the further development of an idea proposed by Johnson in 1997 and that envisaged a different strategy in the treatment of LM. First the surgical margins of the LM are established, as if the lesion was a picture and we are drawing its frame. Next, the lesion is then removed with full assurance that excision is complete.6 The initial proposal involved a square or polygonal excision to facilitate the cutting and orientation of the surgical specimen, but depending on the site of the lesion, rounded or polygonal forms are now possible with the use of photographs or marker sutures to indicate the orientation of the specimen.7-9 It is a simple technique that can be performed by any dermatologist.
Mohs micrographic surgery and other techniques of sequential (stepped) excision with the examination of sections taken from the fresh or paraffin-embedded specimen are of proven efficacy1,3,4,10 but are only performed in specialized centers. In Mohs micrographic surgery, the interpretation of the frozen sections by the pathologist can be very difficult and occasionally the wound must be left open while waiting for the results of examining paraffin-embedded sections.
The technique described in this paper, in which the initial step is to locate the margins, can be very useful in treatment centers where Mohs micrographic surgery is not available or in certain circumstances, such as recurrent tumors with poorly defined borders, older patients or patients living at a distance from the hospital, and lesions whose size means that a flap will be required to close the defect, thereby distorting the margins. The spaghetti technique has several advantages. Routine pathology processing systems can be used and the dermatologist needs no special training. No wounds are left open (meaning that the patient can be discharged without the need for special measures), and there is time to design the reconstruction technique according to the histological findings and the size of the defect, both of which will be known before the final procedure. One of the limitations of this technique is that foci of invasive malignant melanoma cells may be present within the LM, and the excision must therefore reach a deep plane. Another problem is that the complete excision of the lesion will be delayed by days or weeks, and the reason for this must be explained to the patient.
Please cite this article as: García Bracamonte B, Palencia-Pérez SI, Petiti G, Vanaclocha-Sebastián F. Técnica de delimitación del perímetro en el tratamiento quirúrgico del lentigo maligno y el lentigo maligno melanoma. Actas Dermosifiliogr.2012;103:748-750.