To describe the clinical and epidemiological characteristics of syphilis in men who have sex with men (MSM) in an area of Mallorca, Spain.
MethodsWe performed a retrospective analysis of syphilis cases in MSM seen at a hospital in Mallorca between January 2005 and June 2013.
ResultsFifty-five cases of syphilis were recorded in MSM during the study period (34.3% of all cases diagnosed), and 74.5% of these patients had human immunodeficiency virus (HIV) coinfection. The two diseases had been diagnosed simultaneously in 70.7% of this population. Patients with HIV coinfection had a median CD4 count of 456cells/μL (range, 29-979 cells/μL). Syphilis was diagnosed clinically in 49.1% of cases and by screening in the remaining 50.9%. The most common form of syphilis was late latent or indeterminate syphilis (41.9% of cases). In the group of men with syphilis, MSM had a higher risk of HIV infection.
ConclusionsA majority of MSM with syphilis had HIV coinfection. HIV screening is therefore essential in this population and could even result in early diagnosis.
Describir las características clinicoepidemiológicas de la sífilis en la población de hombres que tienen sexo con hombres en un área de Mallorca.
MétodosRevisión retrospectiva de los casos de sífilis en pacientes hombres que tienen sexo con hombres (HSH) entre enero de 2005 y junio de 2013 en un hospital de Mallorca.
ResultadosEncontramos 55 casos de sífilis en HSH, el 34,3% de los casos de sífilis del periodo de estudio. El 74,5% tenían coinfección por el virus de la inmunodeficiencia humana (VIH). El 70,7% de los diagnósticos de infección por VIH y sífilis fueron simultáneos. Los pacientes con infección por VIH tenían una mediana de CD4 de 456 (29-979). Se diagnosticaron por clínica el 49,1% y por cribado el 50,9% de los casos. La sífilis latente tardía o indeterminada fue la entidad más frecuente (41,9%). Los pacientes HSH tenían más riego de estar infectados por VIH que los varones no HSH.
ConclusionesLa mayoría de pacientes HSH con sífilis presentan coinfección por el VIH, siendo por lo tanto fundamental el cribado de VIH en estos pacientes, lo que incluso puede permitir un diagnóstico temprano de la misma.
Syphilis is a universally distributed disease caused by the spirochete Treponema pallidum subspecies pallidum that has important health, social, and economic repercussions. The number of syphilis cases has been increasing in various European and North American cities since the second half of the 20th century.1,2 Men who have sex with men (MSM) account for much of this increase.3–6 A worryingly high proportion of MSM with syphilis are also infected with the human immunodeficiency virus (HIV).3,5,7 The reasons for this change of trend appear to be complex7 but include migratory movements, contacts between different population groups, changes in risky behaviors, the use of various drugs, and the decrease in safe sex practices in MSM that coincided with the introduction of antiretroviral (ARV) therapy.8 In 2011, 3522 cases of syphilis were reported in Spain, and the incidence of the disease was 7.6 cases per 100 000 inhabitants. The annual incidence of syphilis grew considerably between 2005 and 2011.2 The autonomous communities that reported the highest rates were Madrid (14.3 cases per 100 000 inhabitants), the Balearic Islands (11.6 cases per 100 000 inhabitants), and Asturias (10.9 cases per 100 000 inhabitants).2 The aim of our study was to describe the clinical and epidemiological characteristics of syphilis in MSM within the area of influence of our hospital and to compare these characteristics with those of heterosexual men.
Materials and MethodsDesignWe performed a retrospective analysis of the syphilis serologies carried out between January 2005 and June 2013 at Hospital Son Llàtzer, a 350-bed hospital in Palma de Mallorca that serves a population of 225 000 inhabitants. The study was approved by the hospital's research committee.
PatientsAll cases of syphilis confirmed serologically in MSM during the study period were included regardless of the reason for which the serology was ordered (screening of asymptomatic patients or appearance of clinical symptoms).
MethodsAt our hospital, the first step in syphilis screening is a treponemal test that detects antitreponemal antibodies by means of a chemiluminescence immunoassay (CLIA), a test described as having 100% sensitivity and 99.8% specificity.9 In the event of a positive CLIA result, a rapid plasma reagin test (RPR) and a second treponemal test—Treponema pallidum hemaglutination assay (TPHA)—are then carried out to confirm the result of the first test or detect a false positive.
Study VariablesThe following clinical and serologic data were retrospectively collected from the patients’ electronic medical records: age, sexual orientation, smoking and alcohol intake, HIV serology, CD4 cell count, use of ARV therapy, previous diagnosis of syphilis, other sexually transmitted infections (STIs), country of origin, syphilis status, and treatment received.
Definitions- a)
Primary syphilis: Clinical picture (hard chancre accompanied or not by bilateral lymph node enlargement) consistent with positive results in treponemal tests (CLIA, TPHA), regardless of nontreponemal test results.
- b)
Secondary syphilis: Clinical picture consistent with positive results in treponemal (CLIA, TPHA) and nontreponemal (RPR) tests.
- c)
Early latent syphilis: Positive results in treponemal (CLIA, TPHA) and nontreponemal (RPR) tests without clinical symptoms, with evidence of a picture consistent with primary syphilis or seroconversion > 1 year before diagnosis.
- d)
Late latent syphilis or syphilis of unknown duration: Positive results in treponemal (CLIA, TPHA) tests, regardless of nontreponemal test results, without clinical symptoms or prior treatment, and with evidence of syphilis infection > 1 year earlier or unknown duration of infection.
- e)
Neurosyphilis: Clinical suspicion of syphilis affecting the central nervous system and positive serology in the cerebrospinal fluid in either nontreponemal (venereal disease research laboratory) or treponemal (fluorescent treponemal antibody absorption) tests.8
- f)
Serologic cure: 2-dilution RDR titer decrease in patients with positive nontreponemal test results.
- g)
Reinfection: Serologic titer increase following a correct serologic response.
- h)
Treatment failure: Decrease of < 4titers at 6months.
In the descriptive analysis, we determined medians and ranges for continuous variables and frequencies and percentages for categorical variables. Quantitative variables were compared using the t test. For qualitative variables, the χ2 test was used when the necessary applicability criteria were met. Statistical significance was set at a value of P<.05. For risk estimation, odds ratios were calculated with a 95% CI. The statistical analysis was carried out using the SPSS statistical package (version 18) and Epidat (version 3.1).
ResultsDuring the study period, 323 cases of syphilis were diagnosed. In 161 cases (49.8%), the patient's sexual orientation was included in the clinical record: 55 patients (34.2%) were MSM and 106 (65.8%) were heterosexual. Of the heterosexual patients, 39 (36.8%) were men and 67 (63.2%) were women. Although there was some interannual variability, the number of syphilis cases diagnosed per year was relatively stable. The trend over time in the diagnosis of syphilis cases in MSM remained stable throughout the study period.
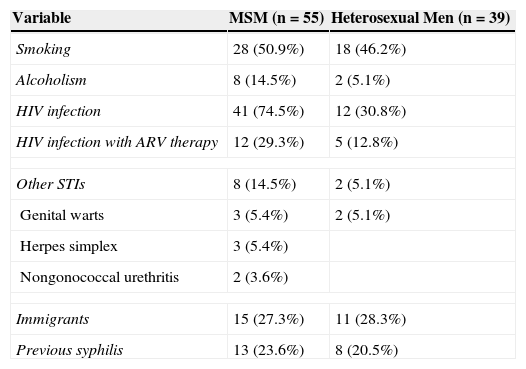
Results in Men Who Have Sex With MenIn MSM patients, the median age was 37.5 years (range, 20-80y). Other epidemiologic variables are shown in Table 1. Serologic status for HIV was known in all cases. Forty-one patients (74.5%) were HIV-positive. Of the HIV-positive patients, 12 (29.3%) were receiving ARV therapy. In the remaining 29 patients, HIV and syphilis were diagnosed simultaneously. In HIV-infected patients, the median CD4 count was 456cells/μl (range, 29-979cells/μl).
Clinical Characteristics of Male Patients (MSM and Heterosexual Men) With Syphilis.
| Variable | MSM (n=55) | Heterosexual Men (n=39) |
|---|---|---|
| Smoking | 28 (50.9%) | 18 (46.2%) |
| Alcoholism | 8 (14.5%) | 2 (5.1%) |
| HIV infection | 41 (74.5%) | 12 (30.8%) |
| HIV infection with ARV therapy | 12 (29.3%) | 5 (12.8%) |
| Other STIs | 8 (14.5%) | 2 (5.1%) |
| Genital warts | 3 (5.4%) | 2 (5.1%) |
| Herpes simplex | 3 (5.4%) | |
| Nongonococcal urethritis | 2 (3.6%) | |
| Immigrants | 15 (27.3%) | 11 (28.3%) |
| Previous syphilis | 13 (23.6%) | 8 (20.5%) |
Abbreviations: ARV, antiretroviral; HIV, human immunodeficiency virus; MSM, men who have sex with men; STI, sexually transmitted infection.
Syphilis was diagnosed clinically in 27 cases (49.1%) and by screening in 28 asymptomatic patients (50.9%). Evidence of previous syphilis infection was present in 13 cases (23.6%).
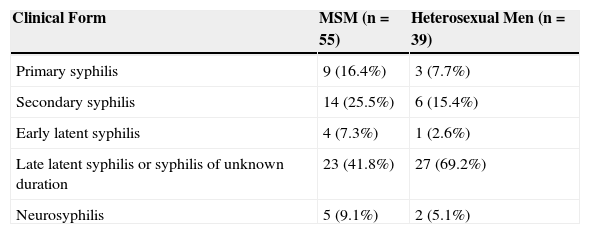
The most frequent clinical form of the disease was late latent syphilis or syphilis of unknown duration, which was diagnosed in 23 cases (41.8%) (Table 2). A total of 50 patients underwent treatment, 48 (96.0%) with penicillin and 2 (4.0%) with doxycycline, although the reason for the use of the latter drug was not indicated in the clinical records. No treatment was carried out in 5 patients with late latent syphilis, and the reason was not indicated in the clinical records. Clinical and serologic cure was achieved in 30 patients (60.0%). Cure was not achieved in 1 case (2.0%) because the patient died for another reason, and the remaining 19 patients (34.5%) were lost to follow-up.
Clinical Stage of Syphilis Cases in MSM and Heterosexual Men.
| Clinical Form | MSM (n=55) | Heterosexual Men (n=39) |
|---|---|---|
| Primary syphilis | 9 (16.4%) | 3 (7.7%) |
| Secondary syphilis | 14 (25.5%) | 6 (15.4%) |
| Early latent syphilis | 4 (7.3%) | 1 (2.6%) |
| Late latent syphilis or syphilis of unknown duration | 23 (41.8%) | 27 (69.2%) |
| Neurosyphilis | 5 (9.1%) | 2 (5.1%) |
Abbreviation: MSM, men who have sex with men.
In heterosexual men, the median age was 47.3years (range, 18-85 y), significantly higher than in MSM (P<.0053). Other epidemiologic variables are shown in Table 1. As in MSM, serologic status was known for all patients in this subgroup. Twelve heterosexual patients (30.8%) were HIV-positive. In HIV-infected patients, the median CD4 count was 422cells/μl (range, 94-1030cells/μl). Syphilis was diagnosed clinically in 12 cases (30.8%) and by screening in 27 asymptomatic patients (69.2%). As in MSM, the most frequent clinical form of syphilis in heterosexual men was late latent syphilis or syphilis of unknown duration, which was diagnosed in 27 cases (69.2%) (Table 2). Seven heterosexual men (17.9%) were lost to follow-up—fewer than in the MSM group, although the difference was not statistically significant.
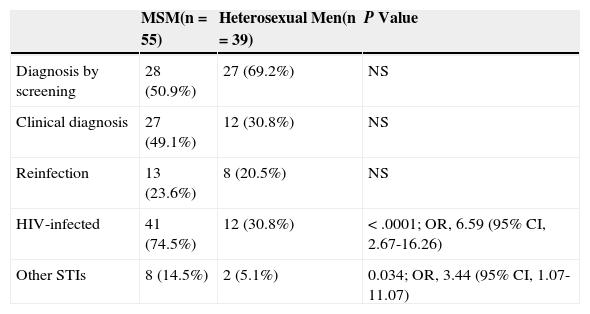
Comparative analysis revealed that HIV coinfection was more common in MSM than in heterosexual men, as shown in Table 3. Although there were no statistically significant differences between the clinical diagnoses and the screening diagnoses (even when each clinical form is analyzed separately), the symptomatic forms of the disease were more common in MSM. The median CD4 count was higher in MSM patients than in HIV-infected heterosexual patients—in whom it was 422cells/μl (range, 23-103cells/μl)—although the difference was not statistically significant.
Comparative Analysis of Syphilis Cases in MSM and Heterosexual Men.
| MSM(n=55) | Heterosexual Men(n=39) | P Value | |
|---|---|---|---|
| Diagnosis by screening | 28 (50.9%) | 27 (69.2%) | NS |
| Clinical diagnosis | 27 (49.1%) | 12 (30.8%) | NS |
| Reinfection | 13 (23.6%) | 8 (20.5%) | NS |
| HIV-infected | 41 (74.5%) | 12 (30.8%) | < .0001; OR, 6.59 (95% CI, 2.67-16.26) |
| Other STIs | 8 (14.5%) | 2 (5.1%) | 0.034; OR, 3.44 (95% CI, 1.07-11.07) |
Abbreviations: HIV, human immunodeficiency virus; MSM, men who have sex with men; NS, not significant; OR, odds ratio; STI, sexually transmitted infection.
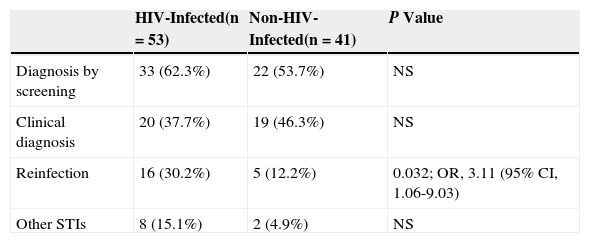
Comparative analysis of HIV-infected men (either MSM or heterosexual) and non-HIV-infected men showed only that syphilis reinfection was more common in the former group (Table 4). Finally, we observed a trend toward a greater prevalence of symptomatic cases in HIV-infected patients, although no statistically significant differences were found, even when patients were analyzed by syphilis status.
Comparative Analysis of Syphilis Cases in HIV-Infected Men and Non-HIV-Infected Men.
| HIV-Infected(n=53) | Non-HIV-Infected(n=41) | P Value | |
|---|---|---|---|
| Diagnosis by screening | 33 (62.3%) | 22 (53.7%) | NS |
| Clinical diagnosis | 20 (37.7%) | 19 (46.3%) | NS |
| Reinfection | 16 (30.2%) | 5 (12.2%) | 0.032; OR, 3.11 (95% CI, 1.06-9.03) |
| Other STIs | 8 (15.1%) | 2 (4.9%) | NS |
Abbreviations: HIV, human immunodeficiency virus; NS, not significant; OR, odds ratio; STI, sexually transmitted infection.
Our study allowed us to obtain an overview of the clinical and epidemiologic characteristics of syphilis infection in the MSM population in our area. The high percentage of patients coinfected with HIV in our case series was noteworthy, as was the number of reinfections. The clinical form diagnosed most frequently was late latent syphilis or syphilis of unknown duration, as would be expected in a population in which screening accounts for more than half of diagnoses. The high percentage of patients lost to follow-up was notable.
In recent years, the incidence of syphilis has increased worldwide1,10 and also in Spain2 and the Balearic Islands specifically. This increase in the incidence of syphilis has occurred mainly in HIV-infected people, particularly MSM.7 Although our study found a stable trend in diagnoses of syphilis in MSM, it must be noted that the study period—from 2005, when the CLIA method of syphilis screening became available, until 2013—was very short.
Most of the worldwide increase in the incidence of syphilis occurred in the late 1990s and the first years of the 21st century, with a linear increase continuing until the present day. This increase has coincided with the introduction of ARV therapy—which allows better control of HIV infection—and a consequent change in risky behaviors brought about by a false sense of protection against potential HIV-related clinical complications.11 In a series of 26 patients in Spain, inconsistent condom use and a larger number of sexual partners were found to be risk factors for syphilis in MSM.12
Because our study was conducted at a hospital—as opposed to a center dedicated exclusively to treating STIs—we have no specific data on risk behaviors. Approximately half of the MSM patients in our series were diagnosed clinically—a notable finding, as one would expect more cases to be diagnosed by screening in this high-risk group. This finding can probably be explained by the fact that the patients included in the analysis were evaluated in a hospital setting as opposed to a primary care center or a center dedicated exclusively to STIs, where screening would be the predominant diagnostic method.
When the MSM population was compared with the population of heterosexual men, the symptomatic forms of syphilis—primary, secondary, and neurosyphilis—were found to be more frequent in MSM, although the differences were not statistically significant. HIV coinfection was also more common in MSM. This finding is consistent with the previous literature,13 although, notably, the percentage of MSM coinfected with HIV was much larger than in other series,4,5,12 including a Spanish multicenter epidemiologic study of more than 500 MSM with syphilis.13 The high percentage of HIV coinfection in our case series—even higher than that found in a Spanish epidemiologic study of hospitalizations for syphilis3—was not limited exclusively to MSM. Because syphilis and HIV share mechanisms of transmission, diagnosis of both infections is not uncommon, especially in groups like MSM that engage in risky sexual practices. In addition, syphilis can enhance transmission of HIV, mainly through mucosal abnormalities caused by genital ulcers.14 The association between syphilis and HIV is therefore of great epidemiologic and clinical importance because both infections are associated with high morbidity and mortality and are therefore public health problems.7,8 HIV infection can also modify the natural course of syphilis infection, and symptomatic infections (secondary syphilis, neurosyphilis) are more common in HIV-infected patients.15 This could explain the larger number of symptomatic syphilis diagnoses in MSM in our study (nearly three quarters of MSM with syphilis were also infected with HIV). This result contrasts with the findings of other international case series in which the percentage of coinfected patients was smaller,16–19 although most of those works were based on studies of population screening.
Remarkably, nearly three quarters of the cases of HIV-syphilis coinfection were diagnosed simultaneously, a much higher percentage than that found in other case series.4,18,20 In these patients, HIV was diagnosed at a relatively early stage (with a median CD4 count of 456), as in previous studies.4 This finding highlights the importance of proper screening for HIV infection in syphilis-infected MSM, which could allow the viral infection to be diagnosed at an earlier stage.
The number of patients lost to follow-up in our study was high—approximately one third of the evaluated population—but lower than the percentage found in other case series.19
The percentage of MSM patients was lower than that found in other Spanish studies, although the earlier works were based on studies carried out in large cities at centers specialized in STIs, where larger aggregations of this risk group can be found.4,5,12
Our study had several limitations. As a retrospective review based on data from clinical records, it was subject to information bias. Additionally, the number of MSM patients was low, probably because many cases with positive serologies for syphilis were excluded from the analysis (latent and treated syphilis were indistinguishable in the patient records). In light of the fact that different societies21–23 have different recommendations regarding screening methods, one possible explanation for this—in addition to the lack of patient follow-up—could be an erroneous interpretation of serologic profiles. Finally, because sexual orientation was recorded in less than half of the clinical histories, a large number of patients were excluded from the analysis.
In conclusion, syphilis-HIV coinfection is very common, especially in the MSM population. The presence of syphilis or HIV should alert the physician to the possibility of the other infection. HIV screening in patients with syphilis, especially MSM, would probably lead to more, and earlier, diagnoses of HIV.
Ethical DisclosuresProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in this article. This document is in the possession of the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gállego-Lezáun C, Arrizabalaga Asenjo M, González-Moreno J, Ferullo I, Teslev A, Fernández-Vaca V, et al. Sífilis en hombres que tienen sexo con hombres: una alarma para la detección de infección por VIH. Actas Dermosifiliogr. 2015;106:740–745.