Few studies have investigated ear involvement in nonsyndromic autosomal recessive congenital ichthyosis (ARCI).
ObjectivesTo assess the type and frequency of otologic manifestations of ARCI in patients under follow-up at the pediatric dermatology department of our hospital.
Materials and methodsWe prospectively studied the presence of ear pain, ear itching, tinnitus, otitis, cerumen impaction, accumulation of epithelial debris, and hearing loss. Daily hygiene measures, topical treatments, medical-surgical interventions, and frequency of visits to an ear, nose, and throat (ENT) specialist were noted in the patients’ medical records. Ear examination and hearing tests were performed in all cases.
ResultsTen patients were studied: 2 had a self-healing collodion baby phenotype and 8 had ichthyosis. There was mention of otologic manifestations in the records of all 8 patients with ichthyosis (100%); 6 of these patients (75%) had abnormalities in the external auditory canal examination and 2 (25%) had conductive hearing loss. Our findings are limited by the small number of patients studied, all of whom were younger than 19 years.
ConclusionsThe involvement of both dermatologists and ENT specialists in the management of patients with ichthyosis is crucial to ensure the application of the best therapeutic and preventive measures. More studies are needed to assess the prevalence and impact on quality of life of ear involvement in patients with ichthyosis and to determine the optimal interval between ENT visits for these patients.
Las complicaciones otológicas asociadas a las ictiosis congénitas autosómicas recesivas (ICAR) no sindrómicas, apenas han sido estudiadas en la literatura.
ObjetivoConocer la frecuencia y el tipo de manifestaciones otológicas de los pacientes diagnosticados de ICAR, actualmente en seguimiento en la unidad de dermatología pediátrica de nuestro hospital.
Material y métodoSe estudió de forma prospectiva la presencia de los siguientes parámetros: dolor, prurito ótico, acúfenos, otitis, tapón de cerumen, acúmulo de restos epiteliales y sordera. Se recogió en la anamnesis las medidas de higiene diaria, tratamientos tópicos o intervenciones médico-quirúrgicas requeridas y la periodicidad con la que los pacientes habían consultado a un especialista de otorrinolaringología (ORL). En todos los casos se realizaron otoscopia y pruebas auditivas.
ResultadosSe estudiaron 10 pacientes, 2 con fenotipo de bebé colodión autorresolutivo y 8 con ictiosis. Un 100% (8/8) de los pacientes con ictiosis referían algún síntoma o signo en la anamnesis, en el 75% (6/8) se observaron anomalías en la exploración del conducto auditivo externo y en el 25% (2/8) se objetivó sordera de conducción, que en un caso se consiguió revertir. Nuestro trabajo está limitado por el escaso número de pacientes, todos menores de 19 años.
ConclusionesEs fundamental la participación conjunta del dermatólogo y del especialista de ORL en el manejo de los pacientes con ictiosis para establecer las mejores medidas terapéuticas y preventivas. Se precisan más estudios que determinen la frecuencia de la afectación otológica, su repercusión en la calidad de vida y la periodicidad mínima idónea de visitas al especialista de ORL.
Nonsyndromic autosomal recessive congenital ichthyosis (ARCI) is a rare hereditary keratinization disorder in which heat intolerance, pruritus, growth abnormalities, ocular and hearing disorders, and social communication deficits may also arise in addition to skin manifestations.1,2 The clinical course of ear complications has rarely been reported in the literature.3,4
ObjectivesThe objective of this study was to determine the type of otologic manifestations present in patients diagnosed with ARCI and currently in follow-up in the Pediatric Dermatology Unit of the University Hospital Son Espases, Spain.
MethodsThe presence of the following manifestations was studied prospectively: pain, ear pruritus, tinnitis, otitis, wax plug, accumulation of epithelial remnants, and deafness. The medical history included daily hygiene measures, topical treatments or medical-surgical interventions required, and frequency of visits to ear-nose-throat (ENT) specialists. All patients underwent otoscopy and hearing tests (pure tone audiometry [PTA], audiometry with visual reinforcement [AVR], and measurement of distortion products in the audiogram [DPgram]). The auditory results were calculated separately for each ear in decibels (dB). The binaural loudness was quantified using pure tone average, which is used in children and recommended by the Bureau International d’Audiophonologie (BIAP). In children who, given their age, could not perform conventional audiometry, estimates were derived from objective tests (DPgram) and behavioral tests (AVR). In these cases, hearing was considered better than 30dB (although the true hearing could be better) when functional hearing was observed.
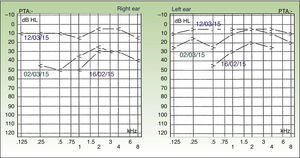
ResultsThe same ENT specialist examined 10 patients, 8 boys and 2 girls, aged between 11 months and 18 years. The underlying molecular deficit was identified in both patients with self-healing collodion baby (TGM1 and ALOX12B) but only in 2 out of 8 patients with skin manifestations of ichthyosis (ALOXE3 and TGM1) (Tables 1 and2). Detailed medical history and the examination performed by the ENT specialist did not reveal otologic symptoms or deafness in either of the 2 cases of self-healing collodion baby. Currently, both have only minimal dermatologic manifestations, although one did have tympanic membrane retraction. All of the remaining 8 children with generalized scaling had some otologic symptom: 8 out of 8 had a history of wax plugs, 6 out of 8 had accumulation of epithelial remnants, 3 out of 8 had ear pruritus, 3 out of 8 had occasional ear pain, 2 out of 8 had otitis, and 1 out of 8 had tinnitus. None of the 8 children used topical ear products daily, only 2 out of 8 cleaned the external auditory canal (EAC) with a cotton wool bud, and 2 out of 8 had been receiving systemic treatment with acitretin for several years. Examination of the EAC of these 8 patients revealed that 2 had wax and epithelial remnants that prevented visualization of the eardrum, 3 out of 8 had scaling with or without wax with normal eardrums, 1 out of 8 had tympanic membrane retraction, and 2 did not have any abnormal findings. The hearing test showed conduction deafness in 2 patients. Ear care, with gradual cleaning and unblocking of the EAC, enabled one patient to regain hearing (case 4, Table 1, Figs. 1 and 2). Of the 10 cases studied, only 3 children had been seen regularly, at least once a year, by an ENT specialist.
Otologic Manifestations of Patients With Nonsyndromic Autosomal Recessive Congenital Ichthyosis.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | |
|---|---|---|---|---|---|---|---|---|
| Molecular Studies | de novo mutation, not previously described, of the ALOXE 3 gene | TGM1, CYP4F22, NIPAL4, ALOXE3, ALOX12B, STS mutations not found. | TGM1, CYP4F22, NIPAL4, ALOXE3, ALOX12B, STS mutations not found. | TGM1 deletion in homozygosis | TGM1, CYP4F22, NIPAL4, ALOXE3, ALOX12B, STS mutations not found. | TGM1, CYP4F22, NIPAL4, ALOXE3, ALOX12B, STS mutations not found. | TGM1, STS mutations not found | TGM1, STS mutations not found |
| Sex/current age | Female/13 years | Male/18 years | Male/12 years | Male/5 years | Male/6 years | Male/10 years | Male/6 years | Male/17 years |
| Pain/frequency | Occasional on contact with water | No | No | No | Occasional | No | No | Occasional on contact with water |
| Pruritus/frequency | No | Yes/monthly | Occasional | Yes/often | Yes/often | No | No | No |
| Tinnitus/frequency | Occasional | No | No | No | No | No | No | No |
| Otitis/frequency | No | No | No | No | Yes/3 times a year | No | No | Yes/annually |
| Treatment if otitis present | Topical and systemic abs | Topical abs | ||||||
| Prophylaxis if otitis present | Avoid contact with water (plugs and cap) | |||||||
| Accumulation of epithelial remnants | Yes | Yes | Yes | Yes | Yes Pineal scaling | No | Yes | No |
| Wax plug/frequency | Yes/bimonthly | Yes/fortnightly | Yes/annually | Yes/annually | Yes/variable | Yes/variable | Yes/variable | Yes/variable |
| Prophylactic treatment if wax plug present | No | No | No | No | No | No | No | No |
| Hypoacusia | No | No | No | ? | ? (at home, repetition requested) | No | No | No |
| Habitual topical treatment | No | No | No | No | No | No | No | No |
| Daily hygiene | Not habitual | Not habitual | Ear cotton wool buds | Cleaning of external scaling remnants | Not habitual | Not habitual | Not habitual | Not habitual |
| Otoscopy | Desquamative EAC (++) normal ear drums | Desquamative EAC (+) normal ear drums | Desquamative EAC (++) wax, normal ear drums | EAC blocked with plugs, eardrums not visible | EAC visible, tympanic membrane retraction | No abnormalities | No abnormalities | EAC blocked with wax and epithelial remnants |
| Audiometry | Normal hearing (PTA) | Normal hearing (PTA) | Normal hearing (PTA) | Conduction hypoacusia most notable in RE (PTA) | Conduction hypoacusia in LE (PTA) | Normal hearing (PTA) | Normal hearing (PTA) | Normal hearing (PTA) |
| Audiometry (in dB) | RE:11; LE: 9; Bi: 10 | RE: 12.5; LE: 14; Bi: 13.5 | RE: 15; LE: 12; Bi: 13 | Initial: RE: 40; LE: 30; Bi: 33; Final: RE: 10; LE: 10; Bi: 10 | RE: 12.5; LE: 41; Bi: 21 | RE: 8; LE: 12; Bi: 9 | RE: 14; LE: 10; Bi: 11 | RE: 12.5; LE: 10; Bi: 11 |
| Frequency of ENT visits | No | Currently none | Annually | Variable frequency | Every 4 months | No | No | No |
| Remarks | Systemic treatment with acitretin since 9 years old | Systemic treatment with acitretin since 11 years old Epistaxis | Recovery of hearing after EAC cleaning | Awaiting completion of hearing study Congenital duplication of distal phalanx of the thumb I | Brother of case 5 | Recurrent tonsillitis |
Abbreviations: abs, antibiotic; Bi, biaural; dB, decibel; EAC, external ear canal; ENT, ear-nose-throat; LE, left ear; PTA, pure tone audiometry; RE, right ear.
Otologic Manifestations of Self-Healing Collodion Baby.
| Case 9 | Case 10 | |
|---|---|---|
| Molecular Studies | Two mutations in heterozygosis in TGM1 gene | Mutation, not previously described, in homozygosis in the ALOX12B gene. TGM1, CYP4F22, NIPAL4, ALOXE3, ALOX12B, STS, ABCA12, and PNPLA1 mutations not found. |
| Sex/current age | Male/11 months | Female/2 years |
| Pain/frequency | No | No |
| Pruritus/frequency | No | No |
| Tinnitus/frequency | No | ? |
| Otitis/frequency | ? | No |
| Treatment if otitis present | ||
| Prophylaxis if otitis present | ||
| Accumulation of epithelial remnants | No | No |
| Wax plug/frequency | No | No |
| Prophylactic treatment if wax plug present | ||
| Hypoacusia | No (family environment) | No |
| Habitual topical treatment | No | No |
| Daily hygiene | Not habitual | Not habitual |
| Otoscopy | No abnormalities | EAC visible, tympanic membrane retraction |
| Audiometry | Normal hearing (DPgram, ARV) | Normal hearing (ARV) |
| Audiometry (in dB) | Threshold <30 | Threshold <30 |
| Frequency of ENT visits | No | No |
| Remarks | Self-healing collodion babyXerosis, increased palmoplantar lines, acral peeling | Self-healing collodion babyPersistent xerosis, increased palmoplantar lines |
Abbreviations: ARV, audiometry with visual reinforcement; dB, decibel; DPgram, audiogram of distortion products; EAC, external ear canal; ENT, ear-nose-throat.
Few studies have assessed the type and severity of hearing loss in patients with ARCI. In 2014, Huang et al.4 published the results of surveys of 135 patients with different forms of nonsyndromic ichthyosis performed using the website of the Foundation for Ichthyosis and Related Skin Types. The results showed that 80% had ear pruritus, 66% had hearing loss, 29% had ear pain, 28% had abnormal hearing test results, and 16% used hearing aids. These manifestations were more frequent in adults (77% in respondents>18 years) than in patients under 18 years of age (53%).
Our study is limited by the low number of patients, all under 19 years of age. However, the fact that it is prospective and that all cases were assessed by the same ENT specialist increases the reliability of the results. In our study, all patients with ichthyosis reported at least 1 sign or symptom in their medical history. In 75%, abnormalities were observed in the EAC examination, and 25% had conduction deafness, which in one case could be reversed thanks to the care routine.
In 2014, Hernández-Martín et al.5 conducted a survey of members of the Spanish Ichthyosis Association to investigate the type and name of the specialists who attended patients with ichthyosis. The study showed that most of these patients were treated by physicians with little experience in ichthyosis and that they are not regularly attended by multidisciplinary teams.
It is necessary to implicate ENT specialists in the management of otologic manifestations associated with ichthyosis and their potential complications.6–8 It is essential that the dermatologist and ENT specialist participate jointly in the management of these patients to establish the best therapeutic and preventive measures (daily hygiene routine, most appropriate topical products). More studies are needed to determine the frequency of otologic involvement, the repercussion on quality of life,9,10 and the minimum ideal frequency for visits to the ENT specialist.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients.
Right to privacy and informed consentThe authors obtained the informed consent of patients and/or subjects mentioned in this article. The informed consent form is located in the archives of the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martín-Santiago A, Rodríguez-Pascual M, Knöpfel N, Hernández-Martín Á. Manifestaciones otológicas en los niños con ictiosis congénitas autosómicas recesivas. Actas Dermosifiliogr. 2015;106:733–739.