Subungual keratoacanthoma is a rare, destructive variant of keratoacanthoma that seldom regresses spontaneously. It may involve the distal tissue under the nail or the proximal nail fold and sometimes also affects the underlying bone. Histopathology is similar to that of other solitary keratoacanthomas but the subungual form shows more pronounced dyskeratosis with little or no nuclear atypia.
We report the case of a 39-year-old Caucasian woman with no relevant past medical history who presented with a very painful hyperkeratotic nodular lesion under the distal portion of the nail of the fourth finger of her left hand; the lesion had grown rapidly during the previous month (Fig. 1). A radiograph of the left hand revealed an osteolytic lesion in the phalanx underlying the nodule. On the basis of these findings we carried out a complete excision of the lesion, adopting a conservative approach with regard to the underlying bone.
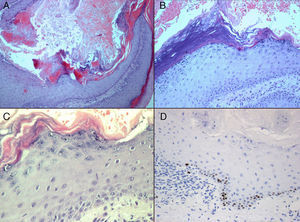
Histopathology using hematoxylin-eosin staining revealed epidermal hyperkeratosis, parakeratotic foci, and a central crater filled with amorphous keratin. Other findings were dyskeratotic cells, a small number of intraepithelial neutrophils and eosinophils, little nuclear atypia, patchy infiltrates of lymphocytes and plasma cells, and little or no fibrosis at the bases of the lesions (Fig. 2a-c). Staining for Ki-67 only revealed positivity in the stratum basale (Fig. 2d). All these findings were consistent with subungual keratoacanthoma.
A, Crater filled with amorphous keratin (hematoxylin-eosin, original magnification ×40). B, Epidermal hyperkeratosis, foci of parakeratosis (hematoxylin-eosin, original magnification ×100). C, Dyskeratotic cells with little nuclear atypia (hematoxylin-eosin, original magnification ×400). D, Positive staining for Ki-67 in the stratum basale.
The differential diagnosis of a painful nodular lesion on the distal phalanx includes dermoid cyst, subungual fibroma, glomus tumor, giant cell tumor of the tendon sheath, digital mucoid cyst, common wart, subungual exostosis, amelanotic melanoma, subungual squamous cell carcinoma (SCC), and subungual keratoacanthoma.1
Subungual keratoacanthoma is a rare, aggressive variant of this tumor which has a higher prevalence in men and a tendency to appear on the first 3 fingers of the hand, particularly the thumb. It consists of a painful, localized endo-exophytic nodular lesion that has a characteristic central keratin-filled crater. Subungual keratoacanthomas differ from typical forms of this tumor in their appearance on hairless skin and the absence of characteristic epithelial cords.2 They tend to be associated less with inflammation and more with deep invasion and a greater number of eosinophilic dyskeratotic cells. The diagnosis should be based on the correlation of clinical, radiologic, and histologic findings.
Subungual keratoacanthoma should be considered in the differential diagnosis of subungual tumors, especially SCCs (Table 1). Radiologically, a subungual keratoacanthoma is almost indistinguishable from a subungual SCC. However, a keratoacanthoma causes a phalangeal lesion with a well-defined border as it expands but does not infiltrate the bone; in addition, keratoacanthomas usually occur in the fifth decade of life, whereas SCCs usually occur in the seventh decade of life. SCCs grow slowly, whereas keratoacanthomas grow rapidly for a few weeks or months before they stabilize and regress spontaneously. If a subungual keratoacanthoma does not regress spontaneously, it can become locally destructive, making differential diagnosis difficult, and cases of malignant transformation to SCC have been reported. The differential diagnosis is currently subject to debate. Some authors believe that these keratoacanthomas are SCCs of low-grade malignancy that can be locally invasive and spread to the underlying bone; however, keratoacanthomas often involute spontaneously.3–5 Recent studies of differences in the expression of certain markers between these 2 tumors (higher expression of Ki-67 and p53 proteins in SCC) that help to establish the diagnosis have concluded that they are separate lesions that behave differently.6,7
Keys to Differential Diagnosis Between Subungual Keratoacanthoma and Squamous Cell Carcinoma.
| Keratoacanthoma | Squamous Cell Carcinoma | |
| Clinical characteristics | Fifth decadeRapid growthSpontaneous regression | Seventh decadeSlow growthNo regression |
| Radiologic findings | Osteolytic lesion with well-defined borders | Poorly-defined borders |
| Histopathologic findings | Symmetric exophytic lesionEpidermal hyperkeratosisCentral crater filled with keratinDyskeratotic eosinophilic cellsLittle nuclear atypiaPatchy dermal infiltration of lymphocytes and plasma cells | Proliferation of epidermal cells with marked cellular and nuclear atypiaAbnormal mitotic figuresInvasion of the dermis and underlying tissues |
| Immunohistochemical characteristics | No increase in Ki-67/p53 expression | Elevated Ki-67/p53 expression |
Therefore, although subungual keratoacanthoma is a rare clinical entity, it is a destructive variant and its differential diagnosis with respect to subungual SCC is essential. Both can present as a painful nodular lesion associated with inflammation and can affect the distal subungual tissue and underlying bone.7–10 Although the 2 conditions can be almost indistinguishable, their prognosis and treatment are different. Subungual keratoacanthoma is treated conservatively, whereas Mohs micrographic surgery is indicated for SCCs that are noninvasive (without bone involvement) and amputation is performed when an SCC has invaded the bone (in cases of rapid growth or delayed diagnosis).11,12
In conclusion, we have reported an unusual case of subungual keratoacanthoma on the fourth finger of a 39-year-old woman, highlighting the importance of considering this diagnosis when SCC is suspected, in the interest of avoiding mutilating treatments.
Please cite this article as: A.J. González-Rodríguez, E.M. Gutiérrez-Paredes, E. Montesinos-Villaescusa, O. Burgués Gasión, E. Jordá-Cuevas. Queratoacantoma digital distal: importancia del diagnóstico diferencial con el carcinoma escamoso subungueal. Actas Dermosifiliogr. 2012;103:549-51.