Lipedematous scalp is a rare condition of unknown etiology characterized by a thickening of the subcutaneous tissue on the scalp. It typically affects the occipital region, and may be accompanied by pain and itching in the affected area. When the condition is associated with hair loss, it is called lipedematous alopecia.1 We report a case of lipedematous alopecia and briefly review the literature.
The patient was a 49-year-old Spanish woman with a history of mild to moderate psoriasis involving both the scalp and the nails since the age of 20 years. She had had surgery for breast cancer (T3 N1 M0) 3 years before this consultation and had been receiving treatment with tamoxifen for about 6 months. She came to our clinic because of severe pain and thickening of the scalp, which had started some 3 months earlier, and more recent hair loss in the occipital region. Three weeks earlier, the patient had visited the emergency department of our hospital complaining of severe scalp pain. A computed tomography scan revealed asymmetry in soft tissue volumes, with significant thickening of the subcutaneous layer (3.12cm) in the vertex and left occipital area (Fig. 1).
On physical examination, the skin of the parieto-occipital area was found to be edematous and boggy, and 2 hairless patches each measuring about 2×2cm and similar in appearance to alopecia areata plaques were observed in the left parietal region. There were also several psoriatic lesions on the scalp, which the patient said had been stable without treatment for several months (Fig. 2).
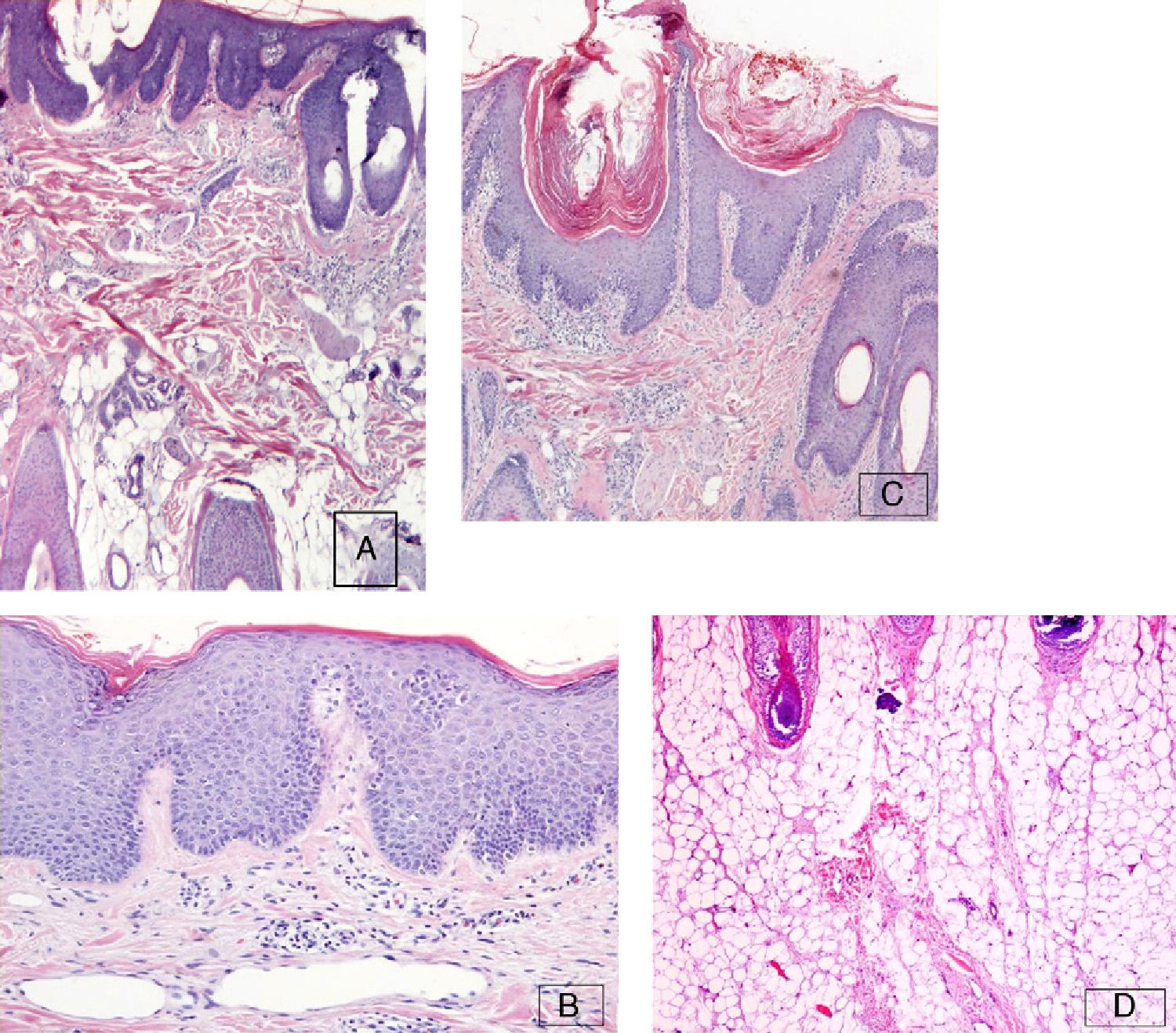
A particularly thick area of the subcutaneous tissue in the left occipital area was biopsied. Histology showed thickened subcutaneous fatty tissue, dermal edema, and a mild perivascular lymphocytic infiltrate in the superficial dermis. There was no evidence of an increase in mucin deposition in the dermis or subcutaneous tissue. Epidermal hyperplasia and keratin plugs in the follicular infundibula were observed. The number of terminal hair follicles in the anagen phase was normal, and dermal blood vessels were telangiectatic (Fig. 3). No significant abnormalities were found in the blood count, biochemistry, antinuclear antibody test, or thyroid profile. On the basis of this evidence, the diagnosis was lipedematous scalp with areas of lipedematous alopecia.
A, Biopsy of the scalp showing the thickened layer of subcutaneous cell tissue with normal follicle morphology (H&E, original magnification x4). B, Epidermal hyperplasia with keratin plugs in the follicular infundibula (H&E, original magnification x20). C, Dilated dermal blood vessels with a telangiectatic appearance (H&E, original magnification x10). D, No evidence of abnormal deposition or panniculitis (H&E, original magnification x10). Abbreviation: H&E, hematoxylin-eosin.
The alopecic plaques and psoriatic lesions were treated with a topical corticosteroid, and hair regrowth was evident within 6 weeks. Oral nonsteroidal antiinflammatory drugs were prescribed for pain control, to be taken as needed.
On follow-up at 9 months, no alopecia was evident, and the pain had lessened considerably. At her final visit, the patient reported that she had had surgery for chronic right-arm lymphedema (a side effect of her breast cancer surgery) with a very satisfactory functional outcome some 6 weeks earlier, and that the scalp discomfort had disappeared entirely.
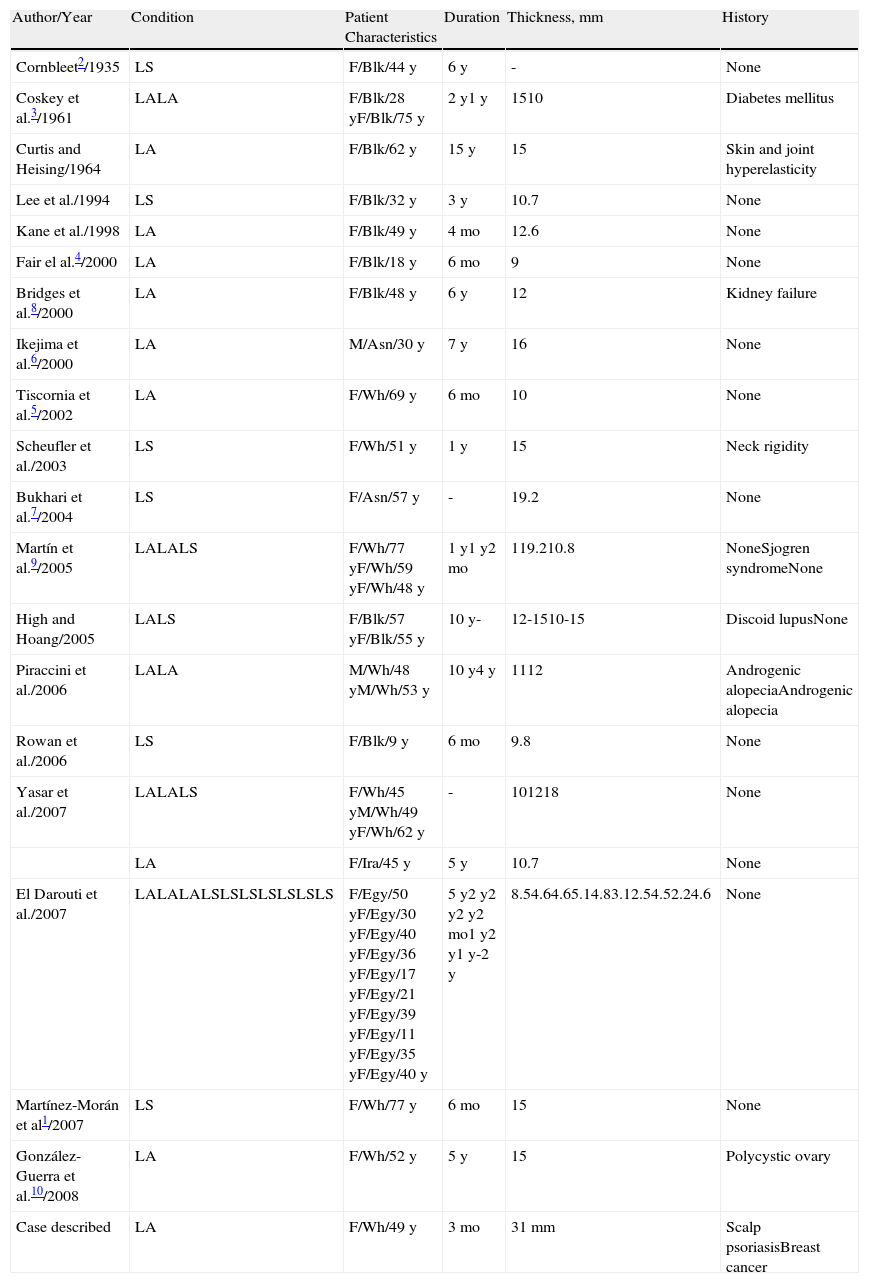
Lipedematous scalp was first described in a black woman in 1935 by Cornbleet.2 In 1961, reporting the cases of 2 black women, Coskey et al.3 coined the term lipedematous alopecia to refer to thickening of the subcutaneous tissue on the scalp coinciding with the inability of the hair to grow more than 2cm. To date only 19 cases of lipedematous alopecia and 16 cases of lipedematous scalp have been reported (Table 1), none associated with any pathology of relevance. In addition to a localized or generalized thickening of subcutaneous tissue, patients may report diffuse pain, numbness, and itching. The thickness of subcutaneous tissue can be measured using ultrasound, magnetic resonance, or computed tomography; a normal thickness in healthy adults is 5.8 ±0.12mm at the bregma. Lipedematous scalp and lipedematous alopecia are probably underdiagnosed; indeed, there is still no agreement on whether they are different processes or simply different stages of the same process.1
Reported Cases of Lipedematous Scalp and Lipedematous Alopecia.
| Author/Year | Condition | Patient Characteristics | Duration | Thickness, mm | History |
| Cornbleet2/1935 | LS | F/Blk/44 y | 6 y | - | None |
| Coskey et al.3/1961 | LALA | F/Blk/28 yF/Blk/75 y | 2 y1 y | 1510 | Diabetes mellitus |
| Curtis and Heising/1964 | LA | F/Blk/62 y | 15 y | 15 | Skin and joint hyperelasticity |
| Lee et al./1994 | LS | F/Blk/32 y | 3 y | 10.7 | None |
| Kane et al./1998 | LA | F/Blk/49 y | 4 mo | 12.6 | None |
| Fair el al.4/2000 | LA | F/Blk/18 y | 6 mo | 9 | None |
| Bridges et al.8/2000 | LA | F/Blk/48 y | 6 y | 12 | Kidney failure |
| Ikejima et al.6/2000 | LA | M/Asn/30 y | 7 y | 16 | None |
| Tiscornia et al.5/2002 | LA | F/Wh/69 y | 6 mo | 10 | None |
| Scheufler et al./2003 | LS | F/Wh/51 y | 1 y | 15 | Neck rigidity |
| Bukhari et al.7/2004 | LS | F/Asn/57 y | - | 19.2 | None |
| Martín et al.9/2005 | LALALS | F/Wh/77 yF/Wh/59 yF/Wh/48 y | 1 y1 y2 mo | 119.210.8 | NoneSjogren syndromeNone |
| High and Hoang/2005 | LALS | F/Blk/57 yF/Blk/55 y | 10 y- | 12-1510-15 | Discoid lupusNone |
| Piraccini et al./2006 | LALA | M/Wh/48 yM/Wh/53 y | 10 y4 y | 1112 | Androgenic alopeciaAndrogenic alopecia |
| Rowan et al./2006 | LS | F/Blk/9 y | 6 mo | 9.8 | None |
| Yasar et al./2007 | LALALS | F/Wh/45 yM/Wh/49 yF/Wh/62 y | - | 101218 | None |
| LA | F/Ira/45 y | 5 y | 10.7 | None | |
| El Darouti et al./2007 | LALALALSLSLSLSLSLSLS | F/Egy/50 yF/Egy/30 yF/Egy/40 yF/Egy/36 yF/Egy/17 yF/Egy/21 yF/Egy/39 yF/Egy/11 yF/Egy/35 yF/Egy/40 y | 5 y2 y2 y2 y2 mo1 y2 y1 y-2 y | 8.54.64.65.14.83.12.54.52.24.6 | None |
| Martínez-Morán et al1/2007 | LS | F/Wh/77 y | 6 mo | 15 | None |
| González-Guerra et al.10/2008 | LA | F/Wh/52 y | 5 y | 15 | Polycystic ovary |
| Case described | LA | F/Wh/49 y | 3 mo | 31 mm | Scalp psoriasisBreast cancer |
Abbreviations: Asn, Asian; Blk, Black; Egy, Egyptian; F, female; Ira, Iranian; LA, lipedematous alopecia; LS, lipedematous scalp; M, male; Wh, White.
Histological findings for lipedematous alopecia are a thickening of the subcutaneous cell tissue, variable dermal edema, a perivascular lymphocytic infiltrate, an absence of abnormal deposition, no evidence of panniculitis, epidermal hyperplasia, and keratin plugs in the follicular infundibula. Terminal hair follicles may be reduced in number or preserved. Dermal blood vessels are often dilated and telangiectatic in appearance.4
The pathogenesis of lipedematous scalp and lipedematous alopecia is unknown. Some authors have suggested that there may be a hormonal factor because most cases are diagnosed in women. Race, once thought to be a key factor, is now considered less important because of the growing number of cases reported in white,5 Asian,6 and Middle Eastern7 women.
One theory proposed to explain hair loss is that the thickening of the subcutaneous tissue may place pressure on the hair follicles, restricting hair growth or shortening anagen cycles.8 Lymph vessels were dilated in our patient, and Martín et al9 reported the same for 2 patients with lipedematous alopecia, suggesting that this effect might play an important role in the pathogenesis of the alopecia. Regarding the association with other systemic diseases, cases have been reported of patients with a history of diabetes mellitus,3 joint and skin hyperelasticity, and acute kidney failure.8
No case has been reported to date of lipedematous alopecia in a patient with comorbid scalp psoriasis or a history of malignancy. Noteworthy in our patient was the intense scalp pain, the very thick subcutaneous layer, the rapid resolution of the alopecic plaques, and the favorable course after surgical treatment of the chronic lymphedema of the arm. Since the patient was already responding to treatment we do not know if the apparently favorable post-surgical response was a coincidence or whether, given the histological evidence of dilated lymph vessels, there was an actual causal relationship between the events.
Please cite this article as: V. Fuentelsaz-del Barrio, V. Parra-Blanco, P. Borregón-Nofuentes, R. Suárez-Fernández. Alopecia lipedematosa concomitante con psoriasis del cuero cabelludo. Actas Dermosifiliogr. 2012;103:551-4.