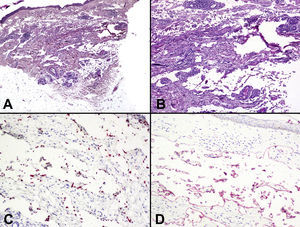
We report on a recent lesion in a 75-year-old woman who had been diagnosed with classic Kaposi sarcoma (KS) 8 years earlier, at which time she presented with plaques on the right thigh and right forearm (Fig. 1A) and no metastasis was detected. Findings from the initial biopsy of the forearm lesions were compatible with nodular KS. During the 8-year follow-up, the patient developed 7 recurrent skin tumors on the forearm and legs. Each tumor had the same clinical appearance in the form of plaques (Fig. 1B), and no systemic involvement was detected at any time. The lesions were treated with liposomal doxorubicin. Biopsies were taken from the forearm at each recurrence and histology continued to show findings consistent with nodular KS mixed with lymphangioma-like areas. These areas were comprised of irregularly-dilated ectatic vascular spaces in the reticular dermis that were lined by moderately atypical endothelial cells. These spaces were greater in number and size than normal lymphatic vessels (Fig. 2). Immunohistochemistry showed strong CD34 positivity. Endothelial cells lining the lymphangioma-like areas of the tumor were also positive on staining with human herpes virus type 8 (HHV-8) antibody (Fig. 2C) and the lymphatic endothelial marker podoplanin (D2-40) (Fig. 2D). Based on these findings, the patient was diagnosed with lymphangioma-like KS. Seven months after completing the most recent cycle of chemotherapy with doxorubicin, the patient presented with a serious recurrence consisting of localized, multinodular, ulcerated lesions on both legs but more severe on the right thigh; severe lymphedema was also noted (Fig. 1C). She was given radiotherapy, second-line chemotherapy with paclitaxel (taxol), and thorough local treatments. At the time of writing the lesions remained ulcerated and had not changed in size. The patient attended scheduled follow-up visits and did not show signs of systemic spread of disease.
A, Initial presentation of the lesion on the flexor aspect of the forearm. Pliable, erythematous-violaceous plaques with poorly defined borders are shown. B, Lesion on the forearm during the fourth recurrence 3 years before development of the most recent lesion. This lesion is indurated and brownish, and the borders of the erythematous plaque are poorly defined. C, Lesion on the right thigh during the recurrence 6 months before the most recently developed lesion. The multinodular tumor is superficial and ulcerated and has a fleshy appearance.
A, Poorly defined dermal tumor comprised of wide vascular spaces. Hematoxylin-eosin, original magnification ×10. B, Dilated vascular lumen located among collagen bundles and lined by a flat endothelium with a benign appearance and without nuclear atypia, cellular pleomorphism, or mitosis. Hematoxylin-eosin, original magnification ×100. C, Nuclei of endothelial cells lining the lumen in the lymphangioma-like areas, stained with the immunohistochemical marker for human herpes virus type 8, original magnification ×200. D, Podoplanin-positive endothelial cells, original magnification ×200.
Lymphangioma-like KS was first described in 1957 by Ronchese and Kern,1 but the histologic characteristics of these tumors were not reported until the 1979 publication of Gange and Jones.2 This tumor is a rare histopathologic variant comprising fewer than 5% of all KS cases and appearing among all KS epidemiological subtypes.3–5
Clinically, the presence of blistering vascular lesions has been described as a characteristic finding in lymphangioma-like KS, although such lesions may also appear in other more common KS presentations.1–7
Histologically, and in contrast with classic KS, the lymphangioma-like variant does not normally have hemosiderin deposits. Red blood cells are found neither outside nor inside the vascular lumen, and spindle-shaped cells are scarce, contributing to the lymphangioma-like appearance of these lesions. As lymphangioma-like areas are typically found at points within a classic KS, the presence of classic KS areas would be an important factor to consider in the diagnosis.4 However, classic KS areas have been absent from some lymphangioma-like KSs, and the differential diagnosis with other benign and malignant vascular tumors is therefore considerably more complex and must include benign lymphangioma, spindle cell hemangioendothelioma, low-grade angiosarcoma, retiform hemangioendothelioma, and targetoid hemosiderotic hemangioma (hobnail hemangioma).2,8,9 Immunohistochemistry with antibodies to HHV-8 plays an essential role in establishing the definitive diagnosis.6,9,10
The histogenesis of KS has been the subject of considerable debate; discussion centers on whether this disease is blood-borne or originates in the lymphatic endothelial cells. With regard to lymphangioma-like KS specifically, histologic findings suggest that it originates from lymphatic endothelial cells, as initially suggested by Gange and Jones.2 This interpretation is consistent with recent immunohistochemical findings showing intense expression of several markers that are specific for the lymphatic endothelium; this was the pattern we saw in the neoplastic cells from our patient. It has been postulated that chronic lymphedema or a history of radiotherapy in the affected area could increase the risk of developing lymphangioma-like KS lesions.1,5 Our patient had never received radiotherapy and did not present with chronic lymphedema. In addition, the lesion in which we detected the lymphangioma-like KS was located on the forearm, not on a lower limb as described in most cases of this type of KS.
This new case of lymphangioma-like KS involved a history of histologically classic KS with successive recurrences consisting of lesions with the same clinical appearance, but with histopathologic findings suggestive of lymphangioma. A detailed histologic study in combination with immunohistochemistry, such as staining for HHV-8 latent nuclear antigen, is essential for correctly diagnosing lymphangioma-like KS.
Please cite this article as: A. Agustí-Mejias, F. Messeguer, A. Pérez, V. Alegre de Miquel. Sarcoma de Kaposi a tipo linfangioma. Actas Dermosifiliogr. 2012;103:547-9.