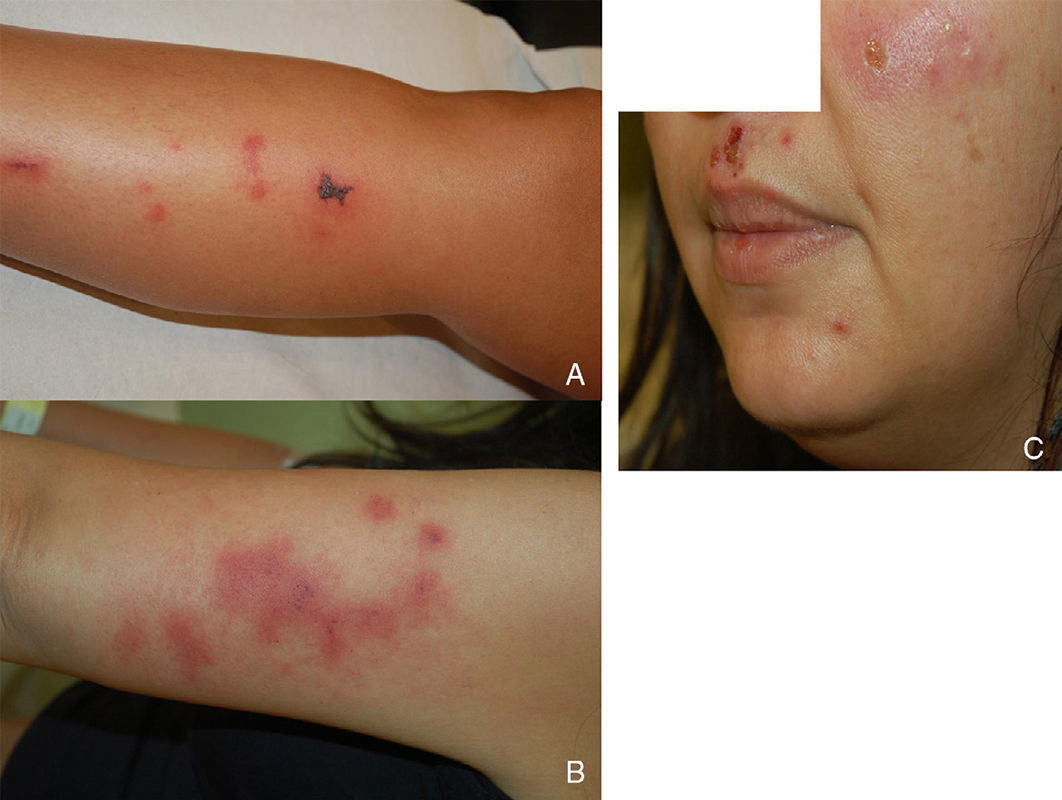
We report the case of a 41-year-old woman with no history of interest who was admitted with lesions that had first appeared 24hours earlier. The lesions took the form of lividoid erythematous violaceous plaques that were retiform in appearance, with necrosis in the center in some cases. They were not painful on palpation and occurred successively on the arms, legs, and face (Fig. 1). The patient also reported pain in the wrists and hands. She was afebrile and denied having taken drugs or toxic substances or being bitten by insects.
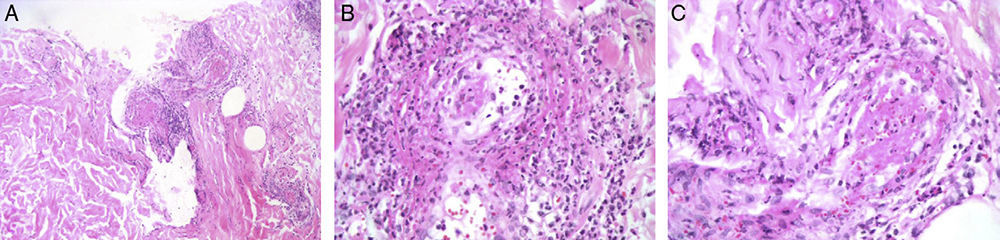
HistopathologyWe performed a skin biopsy (fig. 2), which revealed an inflammatory dermal infiltrate consisting of abundant neutrophilic, polymorphonuclear leukocytes with nuclear remnants in the superficial and perivascular portion. We observed fibrinoid necrosis on the wall and thrombi in small vessels. The blood workup was remarkable for microcytic anemia with increased C-reactive protein levels (71.4mg/L), anti-DNA 70IU/mL, and perinuclear antineutrophil cytoplasmic antibodies (ANCA) 1:640. Urinalysis revealed the presence of cocaine.
What is your diagnosis?
DiagnosisCocaine-associated retiform purpura.
Clinical Course and TreatmentThe patient remained under observation and received systemic corticosteroids in hospital for 48hours. The lesions improved before disappearing some days later. No new lesions appeared.
CommentCocaine is widely consumed, and Spain has one of the highest consumption rates in the world. The drug is often mixed with other substances to increase volume. For many years, the substances used have been mannitol and lactose, local anesthetics, and more active drugs such as paracetamol and caffeine. Levamisole is widely used today and is frequently detected in cocaine throughout the world,1 reaching 70% in the United States. Levamisole is an antihelmintic and immunomodulatory drug that has been associated with the generation of antibodies such as antinuclear antibodies, anti-La antibodies, and ANCAs in patients with a specific immunogenetic profile. It has also been associated with neutropenia and agranulocytosis. It causes purpura on the skin,1–3 affecting mainly the ears, as observed in children who receive the drug to treat nephrotic syndrome.1 Histopathology reveals a mixed pattern of leukocytoclastic vasculitis and microvascular thrombosis that is very characteristic of levamisole.4
The differential diagnosis includes small vessel vasculitis, septic vasculitis, antiphospholipid syndrome, cryoglobulinemia, and necrosis induced by drugs such as ergotamine and cocaine. Wegener granulomatosis (WG) deserves special attention.3,5 A positive cytoplasmic ANCA titer is a highly specific marker of WG.3 There are several reports of patients with midline destructive lesions, together with cutaneous vasculopathy and positive cytoplasmic ANCA titers, which are initially thought to be WG but are eventually associated with consumption of cocaine. Anti-4-hydroxynonenal (HNE) antibodies, a subtype of ANCA, could help to distinguish between both conditions. High anti-HNE titers would point to an association between the clinical findings and consumption of cocaine.4
We report the case of a woman with retiform skin lesions, joint pain, and increased perinuclear ANCA titers who had consumed cocaine. We suggest that her condition could have been caused by the levamisole used to adulterate the cocaine. Our hypothesis is strengthened by clinical, laboratory, and histopathological findings.6 The definitive proof is detection of levamisole in serum or urine, although this is difficult owing to the drug's short half-life, which is only 5-6hours. Cocaine, on the other hand, remains detectable in urine for 4 days. Confirmation is also based on detection of anti-HNE antibodies, although the test may not always available in clinical laboratories.
Dermatologists should become familiarized with the clinical picture of cocaine-associated retiform purpura and be able to recognize this association in order to ensure cessation of the adulterated drug, which is key to satisfactory resolution of the process.
Please cite this article as: Márquez Balbás G, Vidaller A, Tresserra-Casas F, González-Castro J. lacas purpúricas retiformes. Actas Dermosifiliogr. 2015;106:831–832.