A 72-year-old man with a history of ischemic heart disease presented with an asymptomatic lesion in the midchest region. The lesion had appeared as a flat brown plaque a month earlier but had since grown and become ulcerated. The patient denied fever, asthenia, and weight loss.
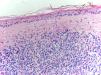
Physical ExaminationThe examination revealed a brownish, indurated, ulcerated 4.5-cm plaque in the midchest region (Fig. 1) accompanied by a nonulcerated satellite lesion with a diameter of 2cm. The peripheral lymph nodes were not palpable.
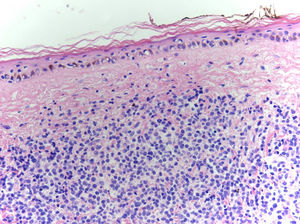
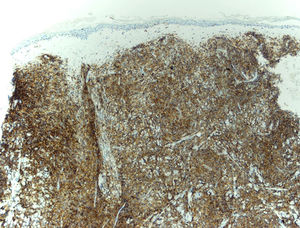
HistopathologyBiopsy of the larger lesion showed a monomorphic, dense, diffuse infiltrate occupying the entire dermis, without extension into the hypodermis. There were no signs of epidermotropism or invasion of adjacent structures or blood vessels. The infiltrate was composed of medium-sized cells with fine chromatin and 1 or 2 nucleoli (Fig. 2). The immunohistochemical study showed positive results for CD4, CD56, CD123, and TdT (Fig. 3) and negative results for other T-cell markers (CD3, CD5, CD8, and perforin). Negative results were also observed for B cell markers (CD20), myeloid markers (myeloperoxidase), and EBER.
Additional TestsPositron emission tomography/computed tomography results were negative except for the skin mass. A bone marrow biopsy and peripheral blood smear showed no extracutaneous involvement.
What Is Your Diagnosis?
DiagnosisBlastic plasmacytoid dendritic cell neoplasm (BPDCN).
Clinical Course and TreatmentInduction therapy was started with idarubicin on days 1 and 2 and cytarabine on days 1 to 5. This was followed by consolidation therapy with intermediate doses of cytarabine at 1 and 2 months. The treatment resulted in complete resolution of the lesions. Maintenance therapy was not administered. There have been no signs of recurrence in the 6 months following treatment initiation.
CommentBPDCN is an aggressive malignant hematologic disease that is included in the 2016 revision of the World Health Organization classification of myeloid neoplasms and acute leukemia.1 It is thought to originate in CD4+ and CD123+ plasmacytoid dendritic cells, although according to a recent study, it might originate in a subtype of CD56+ myeloid dendritic cells.2 It mainly affects elderly males.3
Dermatologists have a key role in the diagnosis of BPDCN, as the tumor starts with skin involvement in 85% of cases.4 The presenting lesions (≤2) are localized in 50% of cases.4 Three clinical forms have been described: nodules (generally localized), ecchymotic macules, and generalized mixed lesions (nodules and macules).4 The initial involvement is exclusively cutaneous in 64% of cases. In the remaining cases, the involvement is extracutaneous and generally affects the bone marrow, spleen, and lymph nodes.4,5 Peripheral blood involvement is detected by the identification of CD4+ CD56+ cells by flow cytometry.
Histologically, BPDCN is characterized by a diffuse infiltrate in the dermis and sometimes the hypodermis. The epidermis is spared. The infiltrate may be perivascular in the initial stages. Angioinvasion and angiodestruction are uncommon findings.5 Cells are medium-sized and have a blastoid morphology. Immunohistochemistry studies tend to be positive for CD4 and CD56 and for the plasmacytoid dendritic cell markers CD123, TCL-1, and CD303. They are negative for myeloid markers, such as lysozyme and myeloperoxidase, enabling differentiation between BPDCN and the main entity in the differential diagnosis: myeloid leukemia cutis. B-cell and T-cell markers are negative.5
Median survival is 15 months.4 Recent data have not shown any differences in survival between patients with localized and generalized BPDCN or between those with and without extracutaneous involvement at diagnosis.4 The treatment of choice is chemotherapy, although radiation therapy is an option for localized disease in elderly patients.3 Chemotherapy regimens used in acute lymphoblastic leukemia have shown the best results to date in BPDCN, with most patients showing complete response.3 Recurrence, however, is the norm and as such allogeneic hematopoietic transplantation is the only curative option for young patients without comorbidities.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-López G, Ceballos-Rodríguez RM, García-Fernández E. Rapidly Growing Lesion on the Chest. Actas Dermosifiliogr. 2018;109:821–822.