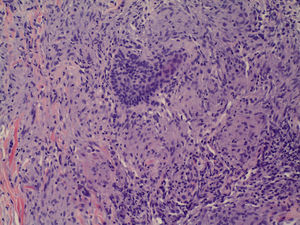
A 62-year-old man with a past history of smoking and systemic hypertension was diagnosed with metastatic nonsmall cell lung cancer with squamous differentiation, with hilar lymph nodes and invasion of the left suprarenal gland. He was therefore started on treatment with docetaxel, which he continued for 2 months before it was withdrawn due to disease progression. He then commenced treatment with nivolumab, 3mg/kg intravenously every 2 weeks. A few days after the second cycle of this drug, the patient developed asymptomatic, erythematous-brownish nodular lesions in the left pectoral region, on the left arm, and in the left scapular region. The lesions coincided topographically with the areas in which the patient had developed varicella-zoster virus reactivation 2 years prior to diagnosis of the cancer and were limited exclusively to the areas of residual scarring from that episode; they thus presented a zosteriform distribution (Figs. 1 and 2). Histology revealed dermal granulomas with no lymphocytic corona or central necrosis, indicating sarcoid-type granulomas (Fig. 3). No multinucleated cells were observed. In view of these findings, extensive blood tests were requested, including angiotensin converting enzyme activity, and a Mantoux test. All the results were normal or negative. No abnormal findings other than those relating to the patient's lung disease were observed on chest x-ray and thoraco-abdominal computed tomography.
Treatment was prescribed with corticosteroids and topical calcineurin inhibitors. Despite this, the lesions persisted unchanged until the patient's death 6 months later; he had continued treatment with nivolumab throughout this period.
Postherpetic granulomatous dermatoses are the most common of the various types of skin reaction that can develop in areas in which varicella-zoster virus reactivation has occurred.1 These dermatoses can arise months or even years after the initial episode of reactivation. Their appearance is related to the concept of the Wolf isotopic response,2 which consists of the development of a new dermatosis at the site of a previous, distinct dermatosis. Various granulomatous dermatoses have been reported: granuloma annulare, granulomatous vasculitis, sarcoid or tuberculoid granuloma, granulomatous folliculitis, and other nonspecific granulomatous dermatoses.3 In all cases, the lesions are limited exclusively to the area affected by the previous herpes zoster, presenting as papules, nodules, or depressed scars.1 The pathogenesis is not fully understood. It is thought that the formation of granulomas may be related to a delayed hypersensitivity reaction to proteins and glycoproteins of the viral envelope,4 rather than complete viral structures5 as, on many occasions, viral DNA is not detected on polymerase chain reaction testing of the granulomatous lesions.6 These reactions have sometimes occurred in patients with lymphoproliferative syndromes,7,8 then being related to changes in the number and function of immunoglobulins, in cellular immunity, and increased hypersensitivity reactions.
Nivolumab is a human monoclonal antibody of the G4 immunoglobulin type. It binds to and blocks the programmed death1 (PD-1) receptor, which is a negative regulator of T-cell activity.9 It is approved for the treatment of metastatic melanoma and squamous cell lung cancer.9 The mechanism of action of nivolumab is similar to that of ipilimumab, another monoclonal antibody used in the treatment of advanced unresectable melanoma; ipilimumab inhibits cytotoxic T-lymphocyte–associated antigen 4, which is a negative regulator of T cells. For this reason, this group of drugs is known as immune check-point inhibitors. The appearance of systemic and cutaneous granulomatous reactions mediated by nivolumab and ipilimumab has been reported on several occasions and is related to their induction of T-cell activation. For example, there has been a case of disseminated granuloma annulare in a patient treated with ipilimumab,10 and several cases of sarcoidosis in patients treated with nivolumab. Those cases presented as a Lofgren syndrome, including infiltrative lesions in cosmetic tattoos,11 with findings including mediastinal lymph nodes and skin lesions,12 or limited to cutaneous sarcoidosis lesions with no systemic involvement.13
After performing additional tests to exclude systemic sarcoidosis, and accepting that sarcoid granulomas can present in numerous diseases other than sarcoidosis, we consider that our patient presented a nivolumab-mediated granulomatous dermatitis secondary to herpes zoster, and that this is the first such case to be reported. We suggest that blockade of the PD-1 receptor by nivolumab stimulates the T cells, promoting hypersensitivity reactions and the formation of granulomas to the proteins of the varicella-zoster virus envelope, thus triggering the postherpetic granulomatous dermatitis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martín-Carrasco P, Pérez-Ruiz C, de Zulueta-Dorado T, Conejo-Mir J. Dermatitis granulomatosa postherpética en un paciente tratado con nivolumab. Actas Dermosifiliogr. 2017;108:783–784.