Skin hyperkeratosis is a common pathology in dermatological consultation. From localized pathology, such as corns or common warts, to diseases with a more diffuse effect such as psoriasis and ichthyosis, diagnosis is usually easy, in response to the history and location of lesions. But sometimes histological or analytical study is essential.
We report a 71-year-old male with multimorbidity (hypertension, diabetes mellitus, ischemic heart disease, mitral regurgitation, left bundle branch block, hepatic steatosis, fibrosing alveolitis, COPD, hypercholesterolemia, hyperuricemia and glaucoma) who presented hyperkeratotic lesions on the legs (Fig. 1). The patient had worked ten years in a photografic laboratory and twenty as carpenter. The lesions were asymptomatic and he had them for more than twenty years. They were located only on the front side of the legs and other skin was respected. Lesions were 2–6mm in diameter and were very adherent. Some had peripheral reinforcement. The patient showed no other symptoms and denied use of cosmetics or chemicals in the area. He had not suffered weight loss or anorexia. He had no history of contact dermatitis, burns or trauma. There was low actinic exposure in the area. No family member had similar injuries. The patient had a history of working in a carpentry workshop for more than twenty years.
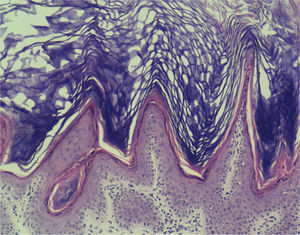
With suspicion of perforating skin disease, actinic keratosis, or porokeratosis, we carried out a 4mm punch of one of the lesions. Histology showed orthokeratotic papillomatosis with focal lymphoid infiltrate in papillary dermis. The sample showed no atypia. The pathology guided us to keratotic lesions with a ‘church spire’ pattern (Fig. 2). This pattern suggests multiple diagnostic possibilities: arsenic poisoning or tars, nutritional deficits (phrynoderma), digitata keratosis, Hopf verruciformis acrokeratosis, or stucco keratosis. Chest radiography was normal but analytical research showed urinary arsenic levels of 317μg/g creatinine (normal levels in occupationally exposed people <100μg/g creatinine). The patient was diagnosed with chronic arsenic poisoning.
Arsenic poisoning has, as its main cause, ingestion of contaminated water.1 This is a significant public health problem in areas of South and Southeast Asia (India, China, Taiwan, Philippines, Thailand, Bangladesh) and the Americas (Argentina, Chile, Mexico, and the USA) where arsenical products are detected either naturally or occasionally by industrial waste. As a second etiologic factor there is workplace exposure. Health damage results from inorganic arsenic (the toxic form) in pesticides, herbicides, mining and galvanized microchips. Occasionally wood preservatives contain arsenic derivatives.2 This could explain our case. Our patient had long worked with wood in a carpentry workshop that, he admitted, was not ventilated. As a final cause we have to consider poisoning or drugs (in traditional Chinese medicine,3 certain antileukemia drugs,4 and, until 1960, Fowler's solution as an antiasthmatic).
Chronic arsenic poisoning has a latency period of years5 before showing clinical signs, but when it does, it may affect multiple systems: cardiovascular (increased QT, T-wave alteration, ST segment alteration), renal and hepatic dysfunction, peripheral neuropathy, blindness, alterations of blood count, electrolytes and acid-base balance, and neoplasms of the lung, bladder, and kidney.6,7 In skin it usually manifests as dotted, symmetrical palmoplantar keratosic lesions of 2–10mm, which may coalesce into plaques. Outside the palms and soles it is characteristic to find mottled pigmentation with hypopigmented areas. It should be noted that there is also increased risk of non-melanoma skin cancer, especially Bowen's disease, in these patients.
Arsenical dermatosis usually shows a pathology with marked hyperkeratosis, scattered parakeratosis, and mild keratinocyte atipia. Adnexal structures are spared while vacuolation of keratinocytes may be noted.
Chelators (dimercaprol and dimercaptosuccinic acid) are used mainly in the treatment of acute poisoning8 but these treatments have proven ineffective in chronic forms.9,10 The use of retinoids has been suggested to prevent the formation of epidermoid carcinomas and Bowen's disease in patients with multiple keratoses. But in chronic forms, the most important action is to avoid toxic exposure, ensuring arsenic-free sources of water and limiting occupational exposure.
Hyperkeratotic lesions, so common in the dermatology consultation, tend to be easily diagnosed. The pattern of injury (location, number of lesions, and form) usually gives us an accurate and rapid diagnosis but occasionally we may have difficulties. In these cases we must take into account less common causes such as congenital forms of hyperkeratosis, perforating diseases, paraneoplastic syndrome, or poisoning. We present this case as a reminder and to illustrate one of those rare cases of pathology that we may see in our medical consultation.
Conflict of interestThe authors declare that they have no conflicts of interest.