Subungual melanoma is uncommon and accounts for just 2% to 3% of all cutaneous melanomas. Less than 10% of subungual melanomas are amelanotic and 90% of these occur on the thumb or great toe. They typically appear in the seventh decade of life and are associated with a delayed diagnosis and a poor prognosis.1–4 Amelanotic subungual melanoma generally manifests as a persistent vascular or ulcerated nodule. On ultrasound (US), subungual melanoma appears as a moderately well-defined hypoechoic area with increased thickness and decreased echogenicity of the nail bed, which frequently erodes into the bone margin of the distal phalanx, viewed as a hyperechoic structure pushing up and eroding into the bilaminar hyperechoic structure of the nail plate. Color Doppler US shows marked hypervascularization. Telangiectatic granuloma is the main entity to be considered in the differential diagnosis. This benign acquired vascular tumor is relatively common, and frequently affects the nail, the nail bed, and the periungual tissues.6 On US, subungual telangiectatic granuloma appears as a focal hypoechoic area with thickening and decreased echogenicity of the nail bed, which pushes up the nail plate but does not erode into the bone margin of the distal phalanx; hypervascularization is also observed.5 Subungual melanoma requires a high index of clinical suspicion given its similarity to other conditions. We report on such a case evaluated at our department.
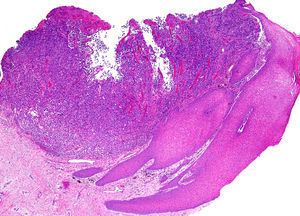
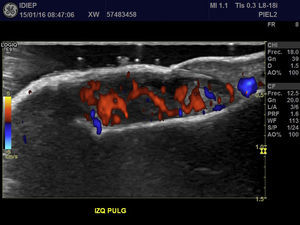
A 67-year-old man presented with a fast-growing asymptomatic lesion of 1 month's duration on the nail of his left great toe. He reported bleeding following minor trauma (Fig. 1). Physical examination revealed a friable subungual erythematous nodule with a vascular appearance associated with disruption of the nail plate. Color Doppler US showed increased thickness and a diffuse decrease in echogenicity of the nail bed. Diffuse hypervascularization of the nail bed was also observed. These findings were consistent with subungual inflammation associated with granulomatous changes predominantly affecting the central zone, suggesting a preliminary diagnosis of telangiectatic granuloma (Fig. 2). The lesion was surgically excised with wide margins, and the histologic evaluation showed nodular, ulcerated malignant melanoma of the nail bed, with a Clark level III, a Breslow depth of 3mm, and a mitotic rate of 10 mitoses/mm2 (Fig. 3).
Amelanotic subungual melanoma generally manifests as a persistent vascular or ulcerated nodule. The differential diagnosis is broad and includes glomus tumor, squamous cell carcinoma, and, most importantly, telangiectatic granuloma.4,7,8 Some of the most main US characteristics that can help to distinguish between these conditions are summarized in Table 1.5
Ultrasound Features of the Main Entities in the Differential Diagnosis.
| Lesion | Echogenicity | Borders | Nail Plate Erosion | Bone Remodelinga | Bone Erosiona | Hypervascularization |
|---|---|---|---|---|---|---|
| Ungual melanoma | Hypoechoic | Poorly defined | +++b | + | +++a | +++ |
| Telangiectatic granuloma | Hypoechoic | Poorly defined | ++ | Rare | + | +++ |
| Glomus tumor | Hypoechoic | Well defined | Rare | +++ | Rare | ++ |
| Squamous cell carcinoma | Hypoechoic or heterogeneous | Poorly defined | +++b | + | ++a | ++a |
Clinically, subungual melanomas have a dull erythematous surface, while the majority of vascular tumors have a bright red surface.9 They also tend to bleed less and grow slowly, over the course of months or years, unlike telangiectatic melanoma, which typically grows in a matter of weeks. There may be a history of trauma in up to 25% of cases of subungual melanoma. The case of amelanotic subungual melanoma described in this report was difficult to diagnose by US, as it lacked well-defined borders and erosion of the bone margin of the distal phalanx, 2 common features of this tumor. In addition, the ability of US to detect pigment is currently limited.
A strong correlation has been reported between tumor thickness measured by color Doppler US and Breslow depth (histology) in cutaneous melanoma, and US is therefore a useful additional tool for investigating suspected cases of subungual melanoma. Although color Doppler US is used to study a wide variety of nail lesions, it has only been used in isolated cases of amelanotic subungual melanoma and none of the studies have used plain US.5
Early studies reported 5-year survival rates of close to 16% for subungual melanoma, and even lower rates were described for patients who had undergone distal amputation at the metacarpophalangeal or metatarsophalangeal levels. Proximal amputation is thus the current treatment of choice.10
Mohs micrographic surgery has also been proposed as a potentially interesting treatment for subungual melanoma. The drawback, however, is that it has been used in small series and more cases are needed to determine its effectiveness.10
In conclusion, amelanotic subungual melanoma is difficult to diagnose both clinically and sonographically. It is therefore essential to rule out other malignant or benign tumors and to perform an early biopsy. Amelanotic subungual melanoma can mimic subungual telangiectatic granulomas on US, particularly in the absence of erosion of the phalanx or nail plate.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Dr Sergio González, dermatopathologist at Pontificia Universidad Católica de Chile.
Please cite this article as: Silva-Feistner M, Ortiz E, Alvarez-Véliz S, Wortsman X. Melanoma amelanótico subungueal simulando granuloma telangiectásico. Correlación clínica, histológico y radiológica. Actas Dermosifiliogr. 2017;108:785–787.