The patient was a 62-year-old Brazilian woman who had been resident in Spain for 3 years. She consulted for pigmented facial spots that had developed progressively over the previous 2 years. She had no past medical history of interest and stated she was not taking any medication. The lesions were asymptomatic and did not give rise to pruritus or pain.
Physical ExaminationThe patient's skin was phototype V of the Fitzpatrick classification. Physical examination revealed poorly defined patches of hyperpigmentation formed of palpable minute grayish papules on a brownish base bilaterally in the malar, zygomatic, temporal, and supraciliary regions. No signs of inflammation or superficial flaking were observed (Fig. 1) and no similar lesions were detected at other sites.
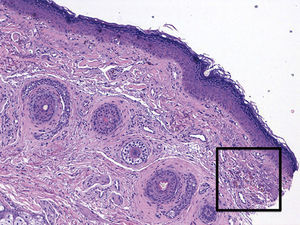
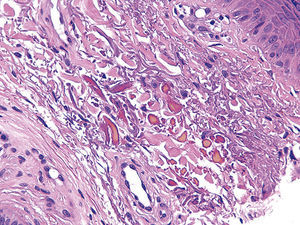
HistopathologyHistology of one of the lesions showed an intact epidermis and the deposition of a dark-yellow material between the collagen fibers in the superficial dermis; the accumulations of this material showed a variable morphology. The adnexa were not affected and there was no inflammatory infiltrate. No signs of melanocyte proliferation or increased melanic pigment in the basement membrane were observed and no melanophages were present in the superficial dermis (Figs. 2 and 3).
No other additional tests were requested.
What Is Your Diagnosis?
DiagnosisHydroquinone-induced exogenous ochronosis.
Clinical courseDuring the diagnostic workup, the patient revealed that for more than 20 years she had been applying a hydroquinone-containing product topically to the facial area to reduce her pigmentation. She was instructed to discontinue using the product and treatment was started with topical retinoids.
CommentThe term “cutaneous ochronosis” was first used by Virchow in 1866 to describe the accumulation of homogentisic acid in the papillary dermis. However, the term was being used in reference to ochronosis secondary to an endogenous pathogenic mechanism in a hereditary disease known as alcaptonuria, in which there is an alteration of the enzyme homogentisate 1,2-dioxygenase.1 It was not until 1975 that Findlay described a form of ochronosis caused by the prolonged use of skin-bleaching creams containing hydroquinone; by the 1980s, this had become the main worldwide cause of exogenous ochronosis.2
Hydroquinone-induced exogenous ochronosis develops due to the prolonged topical application of hydroquinone; onset of the condition is more closely related to the duration of administration than to the concentration of the agent. It most commonly affects phototypes IV and V, which are those in which skin-bleaching treatments are typically used. This prolonged use produces an inhibition of the enzyme homogentisate 1,2-dioxygenase, leading to an accumulation of homogentisic acid in the dermis. Clinically, patients present patches of hyperpigmented papules that resemble caviar eggs; these papules block the follicular openings. The changes are most evident in the area of the zygomatic arches and in the supraciliary region.2 Early stages may only present minimal erythema with mild inflammation. The differential diagnosis should include melasma, which is much more common but does not have papular lesions or follicular plugs, and hyperpigmentation secondary to metal accumulation (pseudo-ochronosis), in which the hyperpigmentation is typically widespread and affects the sclera and mucosas.
The definitive diagnosis is made on histology, confirming the presence of ochre-colored bodies in the superficial dermis, between the collagen bundles; the epidermis and adnexa are not affected. These ochre-colored bodies can adopt different shapes, the most typical being banana-shaped, as can be observed in Figure3 in a biopsy from our patient.3 It is important to remember that these bodies are not arranged around the excretory ducts of the eccrine glands, a feature characteristic of other diseases that are associated with hyperpigmentation but that are not due to the accumulation of homogentisic acid, such as silver accumulation, known as argyria. Pseudo-ochronosis is a more common condition.4
Therapeutically, the first measure is to discontinue the use of hydroquinone. Numerous treatments have been described, including topical retinoids, chemical peeling with glycolic acid, and carbon dioxide laser.5 Currently, the best results are achieved by treatment with the neodymium-doped yttrium aluminium garnet (Nd:YAG) laser, which fragments the ochre bodies and facilitates their phagocytosis.6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Kindem S, Serra-Guillén C, Guillén C. Hiperpigmentación facial parcheada. Actas Dermosifiliogr. 2015;106:317–318.