The appearance of subcutaneous lesions in patients with a history of malignancy nearly always raises diagnostic uncertainty. We present 2 such cases in which ultrasound elastography showed significant differences between one lesion and the other.
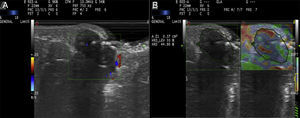
A 55-year-old woman presented with a mildly painful subcutaneous lesion in the periumbilical region that had been present for 10 days. Approximately 4 months earlier, she had been diagnosed with peritoneal carcinomatosis. The neoplastic cells analyzed in the different locations were consistent with adenocarcinoma. Considering the patient's history and the possibility that the mass could be a cutaneous metastasis, we decided to perform an ultrasound examination prior to histologic evaluation. The ultrasound image, captured with a variable-frequency linear probe (8-18MHz), showed a hypoechoic, structurally asymmetric lesion with a well-defined border in the dermis and hypodermis. Doppler color imaging showed slight peripheral hypervascularization. Because these findings were consistent with a possible diagnosis of cutaneous metastasis, we decided to perform strain elastography. The results of the elastogram showed a mean intralesional stiffness of 44.9% (Fig. 1). The corresponding strain ratio was 0.79 and the elasticity score was 2 (of a total of 5). Histopathologic examination ruled out the tentative diagnosis of cutaneous metastasis and showed features consistent with an abscessed retention cyst. The patient was prescribed oral antibiotics, which led to full resolution of the lesion.
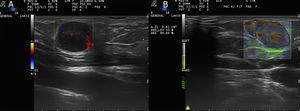
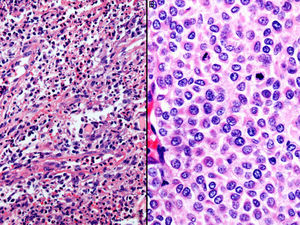
A 45-year-old woman presented with a nodular lesion on the neck measuring approximately 1cm at its widest diameter. Four years earlier, she had undergone surgery to excise a stage T4b superficial spreading melanoma on her right cheek. The staging study showed no evidence of local recurrence or distant spread. Cutaneous ultrasound with an 18-MHz linear probe showed an irregular, hypoechoic structure in the hypodermis. Color Doppler imaging revealed intense intralesional hypervascularization. Although this is a nonspecific finding, it is suggestive of malignancy. According to the strain elastogram, there was a mean stiffness of 84.6% (Fig. 2). The strain ratio was 2.21 and the elasticity score was 3. Unlike in the previous case (Fig. 3A), excision of the lesion and subsequent histopathologic examination with hematoxylin-eosin and immunohistochemical staining confirmed the diagnosis of metastatic melanoma (Fig. 3B).
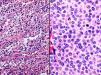
A, Histopathologic image showing abundant macrophages, polymorphonuclear leukocytes, and traces of keratin consistent with a retention cyst (hematoxylin-eosin, original magnification ×40). B, Histopathologic image showing a proliferation of melanocytes with abundant mitotic figures in relation to melanoma metastasis (hematoxylin-eosin, original magnification ×100).
The introduction of ultrasound imaging for dermatologic applications has led to considerable improvements in the diagnosis, treatment, and monitoring of inflammatory and neoplastic diseases in recent years. Ultrasound is a very important tool for the investigation of melanoma as it can assess tumor thickness and vascularization and rule out subcutaneous and lymph node metastases.1 Cutaneous ultrasound can provide key diagnostic information in such cases and also in cases where there is a strong suspicion of melanoma metastasis.2 Irregular hypoechoic nodules with more intense acoustic shadowing in the subcutaneous tissue are highly suggestive of malignancy. These nodules typically have an oval, lobulated, or on occasions, potato-shaped appearance. The above findings, however, are nonspecific and can give rise to false negatives.3,4
Elastography can help when ultrasound does not provide the full diagnostic picture. It has been used to assess liver, breast, and thyroid tissue, but its use in dermatology is relatively new.5 When tissue is subject to pressure applied either mechanically or through an ultrasound beam, it deforms before generally returning to its original shape. Resistance to deformation is a reflection of the hardness or stiffness of a tissue.6 Elastography systems can be classified as strain imaging (based on tissue deformation calculations) or shear wave imaging (based on the characterization of shear wave speed). The 2 main measures used in elastography are stiffness of the target lesion in relation to that of the adjacent parenchyma (strain ratio) and percentage of tissue hardness or stiffness within a lesion.7–9
On analyzing the use of elastography for the diagnosis of primary tumors and lymph node metastases in patients with malignant melanoma, Hinz et al.10 found that elastography combined with ultrasound had greater sensitivity for the detection of lymph node metastases than ultrasound alone. For the elastography study, they correlated findings with patterns of different degrees of elasticity.
In our series, elastography showed evident differences between the 2 lesions (for both strain ratio and percentage of intralesional stiffness), and in addition, the technique was more sensitive than B-mode and Doppler color ultrasound, supporting the findings of Hinz et al.10 Based on the Tsukaba Elasticity Score system, the first lesion, with an elasticity score of 2, had a greater likelihood of being benign than the second lesion (score of 3)
In conclusion, we have provided comparative data from an elastography study of 2 cutaneous lesions in patients with a high risk of malignancy. The differences observed suggest that elastography could provide key diagnostic information when clinical examination and skin ultrasound findings are inconclusive. With the current technology, however, histopathologic confirmation is still required. More studies are needed to determine whether elastography could become a key diagnostic tool for dermatologists.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vilas-Sueiro A, Alfageme-Roldán F, Nájera P, Roustán G. Experiencia de elastografía strain en 2 casos de lesiones subcutáneas sospechosas de malignidad. Actas Dermosifiliogr. 2018;109:274–276.