Extranodal natural killer/T-cell lymphoma (NKTCL), nasal type, is a non-Hodgkin lymphoma that preferentially affects the nasal cavity and paranasal sinuses. The appearance of this disease as a primary neoplasm at other sites, such as the skin, upper respiratory tract, gastrointestinal tract, or testicles, has been reported. Primary NKTCLs of the skin are rare; secondary infiltration of the skin adjacent to a lymphoma arising in the nasal mucosa or in the paranasal sinuses is more common. This is a rare disease, but it has a rapid and aggressive clinical course. It is characterized by central facial lesions that are locally destructive and progress to necrosis. The lack of specificity of the initial clinical characteristics can delay diagnosis.1–5
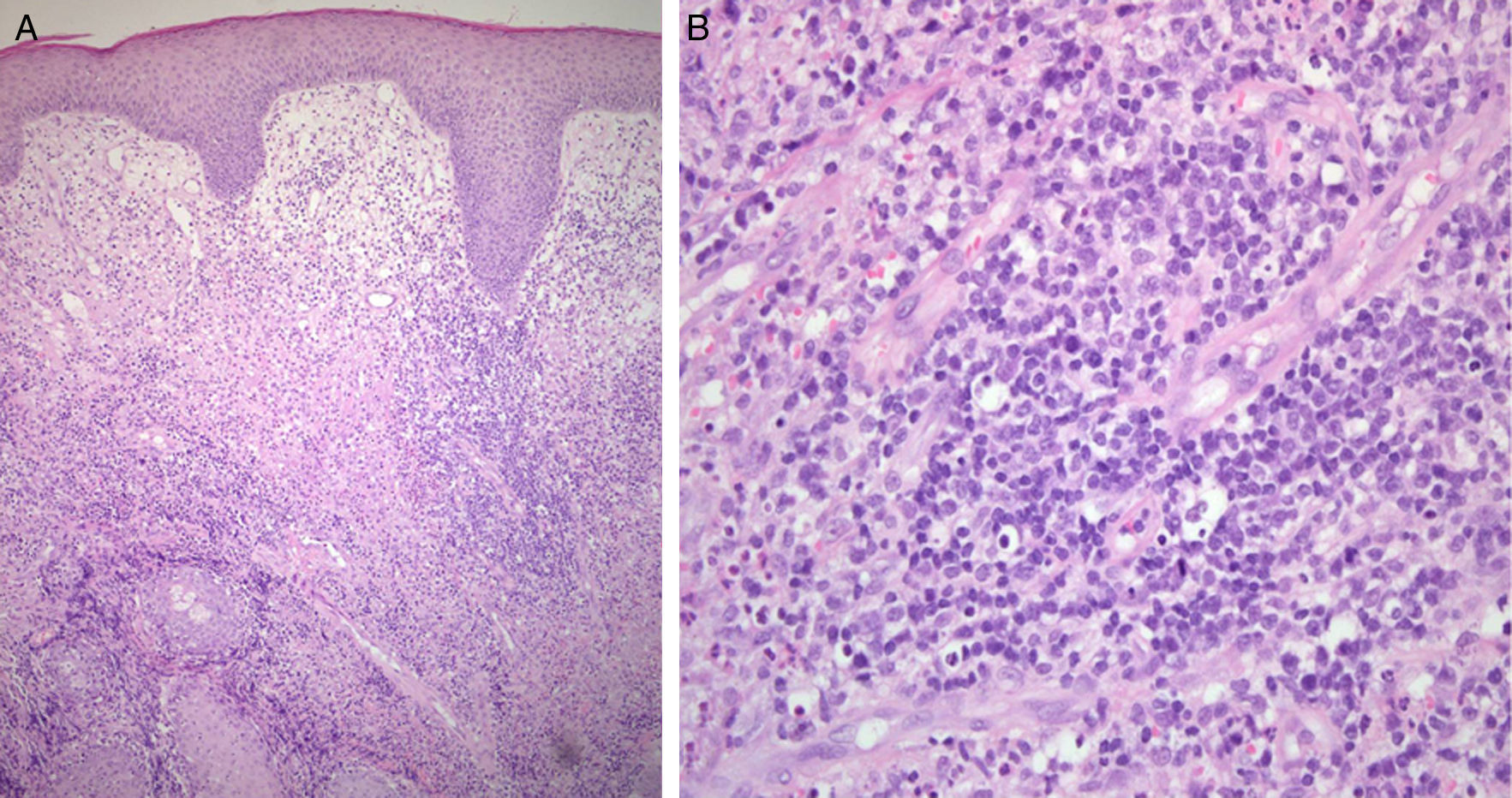
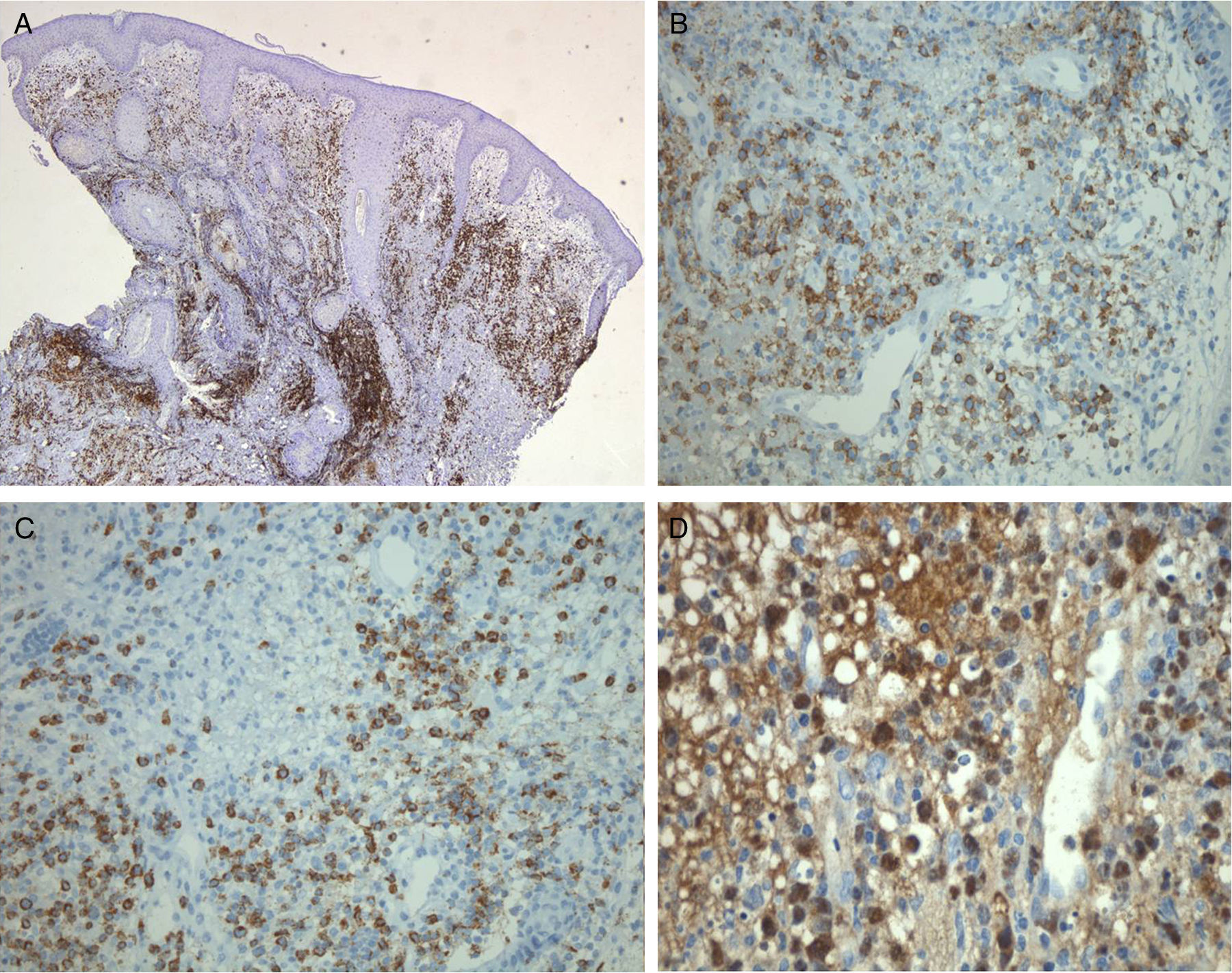
We present the case of a 77-year-old man who reported a 2-month history of right-sided rhinorrhea and rapidly growing skin lesions on the right side of the face. On examination, infiltrated erythematous plaques with well-defined borders were observed on the lower eyelid of the right eye and right cheek (Fig. 1A), and other smaller plaques on the tip of the nose and border of the right nares (Fig. 1B). Histology revealed a dense infiltrate of lymphocytic with atypical morphological features and an angiocentric distribution (Fig. 2, A and B). On immunohistochemistry, there were T lymphocytes positive for CD3, CD56, and granzyme B (Fig. 3, A-C), and the presence of Epstein-Barr virus (EBV) (Fig. 3D) was confirmed on EBER (EBV encoded RNAs) stain. Complete blood count, biochemistry, and bone marrow biopsy were normal. Computed tomography revealed a hypervascular tumor affecting the right orbit, nose, and cheek. Based on these findings we made a diagnosis of stage IA extranodal NKTCL, nasal-type. Despite the early diagnosis and treatment with radiotherapy and chemotherapy, the patient died a year later.
A, Dense lymphocytic infiltrate with a perivascular distribution in the mid and deep dermis, extending partially towards the epidermis and hair follicles. Edematous superficial dermis. Hyperplastic epidermis with preserved architecture and maturation. Hematoxylin and eosin, original magnification×100. B, Population of lymphocytes with scant, pale eosinophilic cytoplasm and atypical nuclei with clumped chromatin and irregular borders. Hematoxylin and eosin, original magnification×400).
A, A CD3+ lymphoid population is present in the superficial and mid dermis, with a notable perivascular distribution. CD3 immunohistochemical stain, original magnification×25. B, Cytoplasm positive for CD56 in the perivascular neoplastic lymphocytic infiltrate. CD56 immunohistochemical stain, original magnification×200. C, Cytoplasm positive for the protease granzyme B, present in activated cytotoxic T-cells and in natural killer cells. Granzyme B immunohistochemical stain, original magnification×200. D, Nucleus of the malignant lymphocytes positive for Epstein-Barr virus mRNA. Epstein-Barr-encoded small RNAs (EBER) stain, original magnification×400.
The term extranodal NKTCL, nasal-type, was first used in the year 2001 by the World Health Organization, replacing the term angiocentric lymphoma.6 Other names by which this disease has been known in the past include lethal midline granuloma, necrotizing midfacial lesion, polymorphous reticulosis, angiocentric immunoproliferative lesion, Stewart granuloma, granuloma gangrenescens, gangrenous proliferative rhinitis, and sinonasal lymphoma. Extranodal NKTCL, nasal-type, accounts for 7% to 10% of non-Hodgkin lymphomas in Asia and South America, but only 1% in Europe and North America. It mainly affects individuals in their fifth decade of life and is more prevalent in men. As in our patient, the disease usually presents initially with rhinorrhea or a purulent nasal secretion, progressing subsequently to lesions with a tendency to ulceration and necrosis secondary to infiltration of the surrounding skin.1–5 The prognosis is very poor, even with early diagnosis, as in our patient, with a mean survival of less than 12 months.1,7
The differential diagnosis must include entities that affect the facial midline, of infectious (Leishmania, paracoccidioidomycosis, histoplasmosis, lepromatous leprosy, mycobacteriosis, mucormycosis), autoimmune (Wegener granulomatosis, lupus), or toxic (cocaine sniffing) etiology.5,8
The etiology of this lymphoma is unknown, but the presence of EBV is an almost constant finding, with detection of viral RNA in the diseased lymphocytes by in situ hybridization using probes marked with Epstein-Barr-encoded small RNAs (EBER); this would suggest a major etiologic and pathogenic role for this virus in the development of this disease.4,5,8 The majority of cells that make up this neoplasm are natural killer cells and peripheral T cells with a cytotoxic phenotype. Histologically, dense infiltrates of atypical lymphocytes are observed in the dermis and subcutaneous cellular tissue. These are small-to-medium sized cells with pale cytoplasm and atypical nuclei with clumped chromatin and irregular borders. There is marked angiocentricity and angiodestruction associated with extensive necrosis. Immunohistochemically, the neoplastic cells are positive for CD2, cytoplasmic CD3, CD56, and cytotoxic proteins (granzyme B, T-cell intracellular antigen [TIA]-1, and perforin).1–5
Treatment of NKTCL is based on radiotherapy for localized disease, though this is usually combined with chemotherapy. If the patient is initially managed using chemotherapy, palliative or coadjuvant radiotherapy is recommended. The poor response to chemotherapy may be due to the expression of multidrug resistance genes. Allogenic bone marrow transplant has been proposed in selected patients. Because of the intrinsically aggressive nature of this type of lymphoma, treatment does not reduce mortality in the majority of cases.9,10
Although this disease is rare in our setting, extranodal NKTCL, nasal-type, must be included in the differential diagnosis of skin lesions that affect the midfacial region and present with nasal symptoms, in order to avoid delayed diagnosis and treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Moreno-Suárez F, Bautista Martínez P, Jiménez Burgos F. Linfoma de células NK/T extranodal nasal. Actas Dermosifiliogr. 2017;108:687–689