Multiple grouped milia or milia en plaque, as it is normally called in the literature, is a rare skin condition of unknown etiology and pathogenesis that is clinically characterized by multiple grouped cysts at a specific site.
We report the case of a 53-year-old Brazilian woman who presented with multiple lesions and mild pruritus that had appeared 6 weeks earlier on both ear lobes. She had been living in Spain for 8 years, had no relevant past medical history, and was receiving no regular treatment. She reported no history of injury, burns, dermabrasion, or use of cosmetics or topical drugs at the site of the lesions.
Physical examination revealed multiple grouped, smooth, yellowish-white cystic lesions, measuring 0.1 to 0.2cm in diameter, with a faintly erythematous surface, on the right helix and ear lobe (Fig. 1). Lesions of similar characteristics were observed on the left ear lobe, but in smaller numbers.
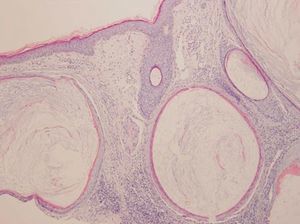
Biopsy of the lesions on the right ear lobe showed multiple follicular infundibular cysts with a perifollicular foreign body–type granulomatous infiltrate response. The cysts were lined with squamous epithelium with a granular layer and slightly basophilic lamellated keratin (Fig. 2).
Based on these clinical and pathologic findings, we diagnosed milia en plaque.
The patient received 4 sessions of photodynamic therapy (PDT) with methyl aminolevulinate hydrochloride cream at 2-weekly intervals. There was a marked reduction in the number of cysts and response was maintained at 5 months (Fig. 3).
Milia are small epidermoid cysts located in the superficial dermis that present clinically as smooth, round white to yellowish lesions. They are classified as primary if they arise spontaneously and are of unknown etiology, and as secondary if they appear in response to repeated trauma, burns, radiation therapy, topical corticosteroids or topical 5-fluorouracil, oral ciclosporin, or other types of aggression.1
Milia en plaque is a rare type of primary milia that was first described in 1903 by Blazer and Bouquet.2 The etiology and pathogenesis of this rare variant are unknown, although associated cases of pseudoxanthoma elasticum and discoid lupus erythematosus have been reported.3,4 The condition is more common in middle-aged adults, with a certain predominance in women.5
Milia en plaque is characterized clinically by the presence of multiple grouped asymptomatic milia within a plaque in a specific location. The most common site is the retroauricular area (with a unilateral or bilateral distribution), but there have been some cases reported in other locations, including the ear lobes, the preauricular region (bilateral distribution), the eyelids, the paranasal region, the supraclavicular region, the submandibular region (bilateral distribution), the back of the hands, and the legs.6
Histologic features include numerous small cavities filled with lamellated keratin, lined by a wall of 2 or 3 layers of epithelial cells. A mild or moderate, predominantly lymphocytic, inflammatory infiltrate with a nonlichenoid pattern is generally observed in the dermis.
The differential diagnosis should include secondary milia, lichen planus follicularis tumidus, comedo nevus, trichoadenoma, Favre-Racouchot nodular elastosis, follicular mucinosis, folliculotropic mycosis fungoides, and steatocystoma multiplex.
Treatment is not fully established but electrodesiccation, dermabrasion, cryotherapy, surgical resection, etretinate, carbon dioxide laser treatment, topical retinoids, oral minocycline and doxycycline, and PDT have been used.1,7–10 Stefanidou et al.1 were the first to use PDT on milia en plaque, obtaining a partial response after 3 sessions at weekly intervals; response was maintained at 1-year follow-up. PDT is based on the photooxidation of biological materials induced by a photosensitizer (5-aminolevulinic acid or topical methyl 5-aminolevulinate), which is selectively retained in specific cancer cells or tissues that are destroyed when exposed to a sufficient dose of light at an appropriate wavelength. It is effective in the treatment of actinic keratosis, basal cell carcinoma, and Bowen disease.
We have described a new case of milia en plaque, which involved both ear lobes and in which PDT led to a significant reduction in the number of cysts. It is the second case in the literature that reports the use of this therapy.
Please cite this article as: Muñoz-Martínez R, et al. Quistes miliares múltiples agrupados. Actas Dermosifiliogr. 2013;104:638–40.