Photodynamic therapy (PDT) is a noninvasive treatment that combines a light source with a topical photosensitizing agent. The technique is widely used in dermatology for treating certain oncologic conditions such as actinic keratosis and superficial basal cell carcinoma. While PDT is safe and effective, an appreciable number of patients present local adverse effects such as erythema, pain, and edema at the treatment site. Isolated incidents of other adverse effects have been described, including transitory hyperpigmentation, cellulitis, and, more rarely, milia.
A 91-year-old man with skin phototype II on the Fitzpatrick scale and a past history of hypertension and hypertensive heart disease visited our department with lesions in the parieto-occipital region of the scalp. The lesions had appeared 3 years earlier and had not improved despite months of keratolytic therapy. Physical examination revealed multiple soft keratotic crusted papules grouped in the parieto-occipital region of the scalp. Shave biopsy of one of the lesions revealed acanthosis with hyperkeratosis, alternating orthokeratosis and parakeratosis, and focal atypia of keratinocytes in the lower third of the epidermis, confirming the suspected diagnosis of actinic keratosis. PDT was performed using 5-aminolevulinic acid hydrochloride gel (78mg/g). The area to be treated was covered with an opaque dressing for 3hours. The area was cleaned using saline solution and exposed to a lamp with red light-emitting diodes at a wavelength of 630nm (Aktilite CL128, Galderma) and the dosage recommended in the product information sheet (37J/cm2). The patient presented considerable erythema in the treated area at the end of the treatment session.
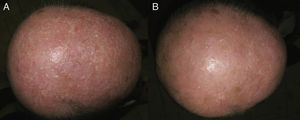
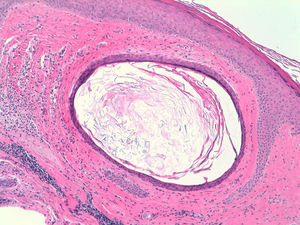
By the follow-up visit a month after treatment, the actinic keratosis had completely resolved; however, multiple millimeter-sized monomorphous, whiteish papules were observed in the treated area (Fig. 1 A). In light of the suspected diagnosis of milia, a 4-mm punch biopsy was performed. The results of histopathology were compatible with milia: multiple cyst-like structures lined by squamous epithelium with a granular layer and containing orthokeratotic keratin (Fig. 2). Treatment was started with 5% salicylic acid in petroleum jelly, applied once daily, and the lesions improved after 2 months of treatment (Fig. 1B).
Milia are small epidermal cysts that present as firm whiteish papules with a diameter of less than 3mm; they are thought to originate in the pilosebaceous follicle. Cysts are classed as primary milia when they appear spontaneously, predominantly on the face, and as secondary milia1 when they are caused by trauma or occur in association with inflammatory skin conditions. Secondary milia have been reported in association with second-degree burns, radiotherapy,2 porphyria cutanea tarda, and after tattooing.3 In our case, the most plausible explanation for the milia may be the intense inflammatory reaction our patient presented during the treatment session.
The appearance of milia following PDT is a rare adverse effect that we had not previously observed in our extensive clinical experience. This phenomenon is known to reflect the severity of phototoxic damage and disruption of the dermal-epidermal junction.4 Milia have been reported in the literature in 3 patients 3 months after PDT (5-aminolevulinic acid hydrochloride). In 2 of the cases, spontaneous resolution was observed after 6 months5 (Table 1).
Cases of Milia Following Photodynamic Therapy Published in the Literature.
| Cases | Age | Phototype | Disease | Location | Photosensitizing Agent | Incubation Time | Lamp | Dose Regimen | Post-PDT Reaction | Clinical Course and Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 Buinauskaite et al. | 68 | III | AK grade I-II | Parieto-occipital | 5-aminolevulinic acid hydrochloride, 20% | 4 h | Curelight (PhotoCure) | 70 J/cm2 | Not available | Spontaneous remission after 6 months |
| Patient 2 Buinauskaite et al. | 77 | III | AK grade I-II | Parieto-occipital | 5-aminolevulinic acid hydrochloride, 20% | 4 h | Curelight (PhotoCure) | 70 J/cm2 | Not available | Spontaneous remission after 6 months |
| Patient 3 Buinauskaite et al. | 84 | III | AK grade I-II | Parieto-occipital | 5-aminolevulinic acid hydrochloride, 20% | 4 h | Curelight (PhotoCure) | 100 J/cm2 | Not available | Persistence of milia No treatment |
| Patient 4 Flores et al. | 91 | II | AK grade I-II | Parieto-occipital | 5-aminolevulinic acid hydrochloride, 7.8% (Ameluz) | 3 h | Aktilite CL128 (Galderma) | 37 J/cm2 | Erythema | Improvement with 5% salicylic acid after 2 months |
Abbreviations: AK, actinic keratosis; PDT, photodynamic therapy.
In our case, in contrast to the 3 cases mentioned above, onset of milia occurred earlier and the condition resolved more quickly following keratolytic treatment. This difference may be linked to the severity of the inflammatory reaction our patient presented after treatment. As in the cases mentioned above, the milia appeared following the application of topical 5-aminolevulinic acid hydrochloride in actinic keratosis. No similar reactions have been reported to date in cases in which the photosensitizing agent was methyl aminolevulinate. This phenomenon may be explained by the greater affinity of 5-aminolevulinic acid hydrochloride for cancerous tissue,6 which leads to greater collateral damage of healthy tissue.
Paradoxically, PDT is one of the most commonly used treatments for milia en plaque.7
We present a new case of milia following treatment of actinic keratosis using PDT. The patient had no past personal or family history of milia. Given the benign and potentially self-limiting nature of the condition, it is important for dermatologists to be able to identify milia and avoid mistaking it for treatment failure. In our case, although we explained that the condition was benign, the patient stated that he was unhappy with the cosmetic result and we therefore started mild keratolytic treatment with very good results.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Flores-Climente V, Dalmau J, Puig L. Milia, una reacción infrecuente tras terapia fotodinámica. Actas Dermosifiliogr. 2019;110:71–74.