Venous ulcers are the main cause of chronic leg ulcers. They have a high prevalence, high morbidity, and a marked socioeconomic impact. Venous ulcers are frequently encountered in dermatology and vascular surgery consultations, require long-term treatment, and commonly recur.1 Compressive therapy is the treatment of choice. However, these ulcers can often become chronic and fail to respond to multiple local treatments and dressings. If a significant improvement is not observed within 4 to 12 weeks, conservative treatment is unlikely to result in cure.2
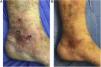
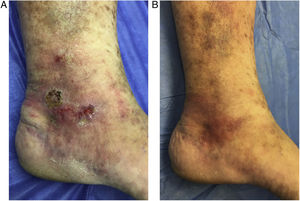
We describe the case of a 69-year-old man, with no medical history of interest, who was seen for a painful venous ulcer on the ankle that had appeared 6 months earlier. The patient had undergone conservative treatment with a compressive bandage and local wound treatment, and had twice received oral antibiotic treatment for superinfection. Physical examination revealed an internal inframalleolar ulcer of 4 cm and 2 adjacent incipient lesions (Fig. 1A), as well as varicose veins with secondary dermatosclerosis and skin hyperpigmentation. Triplex ultrasound (3–13-MHz probe) revealed incompetence of the great saphenous vein, with tributaries projecting towards the ulcer bed, and an adjacent incompetent perforator vein. Ultrasound-guided sclerotherapy of the ulcer bed was performed using the terminal interruption of the reflux source (TIRS) technique. In total, the patient underwent 4 sessions at 1-week intervals using a mixture consisting of 1 part 1% polidocanol foam (0.5mL per session) to 4 parts CO2O2 (Tessari method). Complete re-epithelialization was observed by the fourth week (Fig. 1B). The great saphenous vein was simultaneously ablated by intravenous laser (VascuLife, 1470 nm) to treat the proximal reflux and prevent ulcer recurrence. Six months after treatment the patient remains asymptomatic with no lesion recurrence.
Foam sclerotherapy was proposed as a first-line treatment for venous ulcers in 2004.3 The TIRS technique consists of the treatment of incompetent veins in close proximity to the ulcer bed to generate a sort of internal compressive bandage.4 At the first consultation Doppler ultrasound is performed to examine the vessels of the ulcer bed and to map the venous system. The target vessels are the incompetent perforators and the incompetent veins of the ulcer bed with continuity with the source of the reflux. Foam sclerotherapy is performed and a compressive bandage applied until the next session. Sessions are carried out at weekly intervals until all incompetent target vessels have been obliterated.
In the cases described in the literature TIRS is effective in almost 90% of cases, with a mean healing time of 4 to 8 weeks.4,5 We reported comparable outcomes in a series of 6 clinical cases.6 Compared with conservative treatments or treatment of proximal reflux by sclerotherapy alone, TIRS appears to be a more effective technique, with a shorter healing time.6–9 The beneficial effects of foam sclerotherapy have also been demonstrated in several studies of large series of patients with long-term follow-up. Because it directly targets the source of the venous ulcer, foam sclerotherapy offers better outcomes than other therapies with low quality of evidence ratings, such as venotonic drugs, stem cells, and growth factors. The risk of recurrence appears to be lower than that reported for the treatment of proximal reflux alone.4,6,7 However, the importance of compression stockings or bandages in preventing venous ulcers should not be overlooked.
TIRS can be performed on an outpatient basis, and improvements in ulcers and associated clinical signs can be observed within 2 weeks. The most feared complication is accidental perforation of the posterior tibial veins and consequent thrombosis. The most commonly described adverse effects are pain, bruising, and discomfort caused by the bandages applied after treatment. Other less commonly reported complications of sclerotherapy include transient neurological adverse effects, intra-arterial injection and subsequent ischemia, pulmonary thromboembolism, and deep-vein thrombosis.
We believe that TIRS is a promising and safe technique with a minimum recovery time.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mendieta-Eckert M, Azpiazu-Macho JL, Landa-Gundin N. Tratamiento de úlcera venosa refractaria mediante la «interrupción terminal de la fuente de reflujo». Actas Dermosifiliogr. 2019;110:74–75.