Lichen sclerosus is a rare, chronic inflammatory skin disease that affects the genital and extragenital regions. It was first described by Hallopeau in 1887 as atrophic lichen planus.1 The current most widely accepted term for the disease is lichen sclerosus. We report a case of lichen sclerosus in which lesions appeared only in a previously irradiated area.
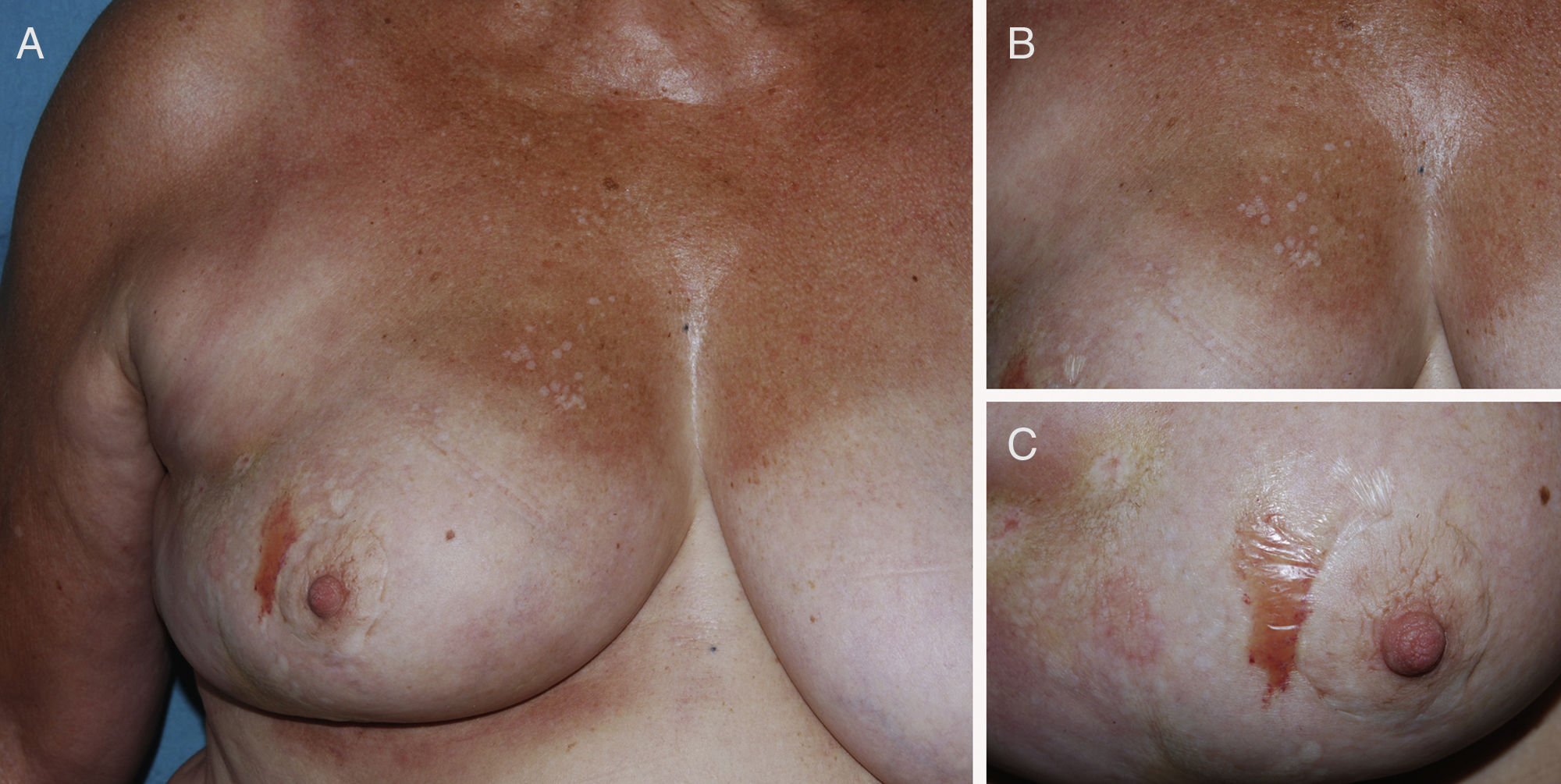
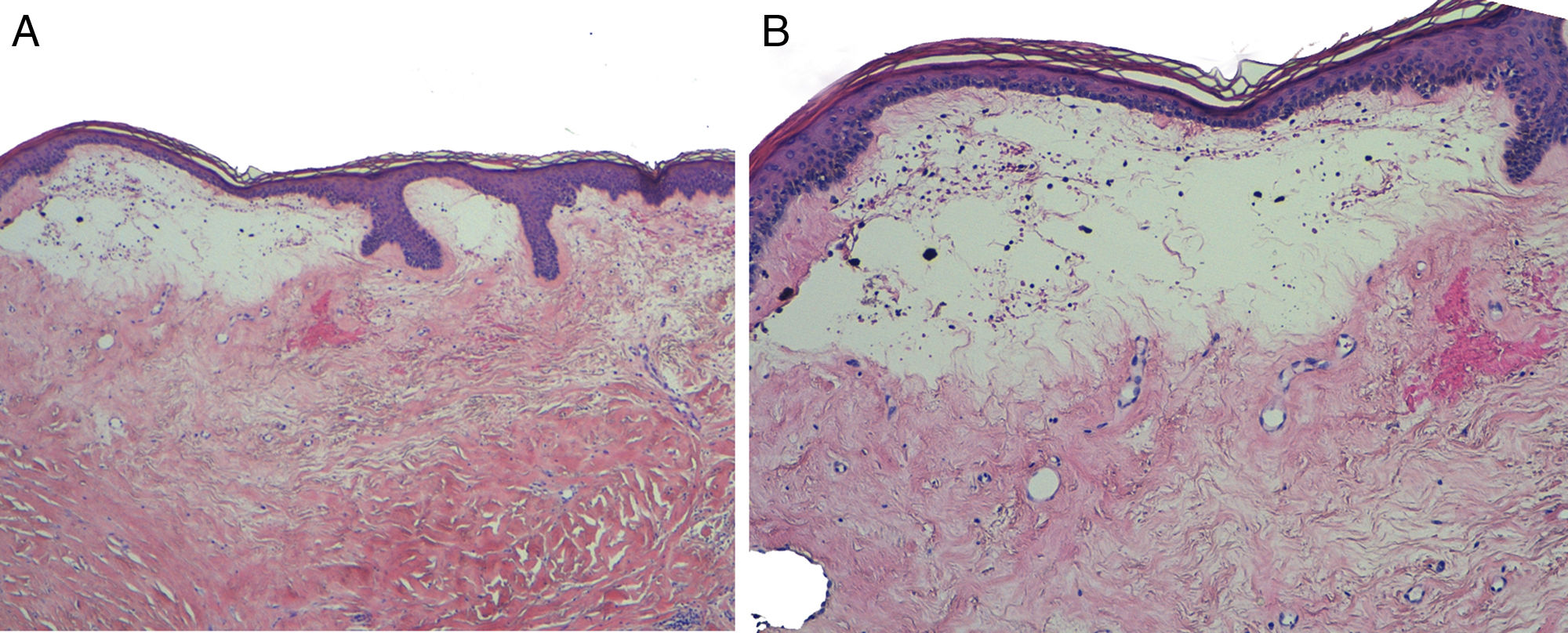
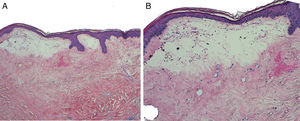
The patient was a 71-year-old woman who had been diagnosed 2 years earlier with an infiltrating lobular carcinoma in the right breast. The tumor was treated with lumpectomy and subsequent radiotherapy. The patient was undergoing treatment with letrozole. Two years after radiotherapy, the patient was referred to us with asymptomatic lesions that had appeared 2 months earlier on the irradiated breast. The physical examination revealed a flaccid blister containing serosanguineous fluid beside the areola of the right breast and small, round, pearly white macules on the right hemithorax and the outer quadrants of the right breast (Fig. 1). The patient presented no associated genital lesions. In light of the suspected diagnosis of lichen sclerosus secondary to radiotherapy, we performed a biopsy of the site of the blister. Histopathology revealed epidermal atrophy and marked dermal hyalinization associated with superficial edema, compatible with lichen sclerosus (Fig. 2A). Secondary subepithelial vesiculation, responsible for the blister, was also observed (Fig. 2B). Treatment was started with daily application of 0.1% topical tacrolimus, which attenuated the whiteish macules and resolved the blister completely. No subsequent new lesions appeared.
The exact prevalence of lichen sclerosus is unknown. It is markedly more frequent in females and may appear at any age, although peak incidence occurs around the fifth and sixth decades of life. Genital involvement is most frequent (85% of cases), concomitant extragenital involvement can be found in up to 20% of cases, and exclusively extragenital involvement is found in up to 2.5%.2
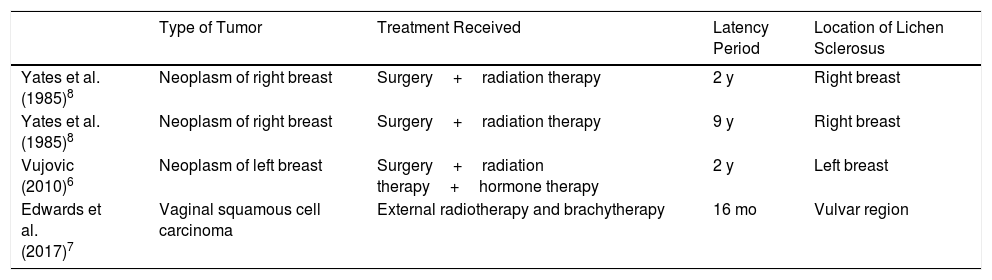
The etiology is unknown, although there appears to be some genetic predisposition. A link with underlying autoimmune mechanisms has also been postulated, as cases have been reported in association with diseases such as vitiligo, alopecia areata, and thyroiditis. What is clear is the presence of the Koebner response in this disease. Cases of lichen sclerosus have been reported in association with jellyfish stings,3 subcutaneous insulin injections,4 and chronic pressure sores.5 The Koebner response may explain the appearance of lesions in previously irradiated areas, as in our case. Although radiotherapy is currently widely used, only 4 cases of lichen sclerosus induced by radiotherapy have been described in the literature (Table 1).6–8
Cases of Lichen Sclerosus Induced by Radiation Therapy Reported in the Literature.
| Type of Tumor | Treatment Received | Latency Period | Location of Lichen Sclerosus | |
|---|---|---|---|---|
| Yates et al. (1985)8 | Neoplasm of right breast | Surgery+radiation therapy | 2 y | Right breast |
| Yates et al. (1985)8 | Neoplasm of right breast | Surgery+radiation therapy | 9 y | Right breast |
| Vujovic (2010)6 | Neoplasm of left breast | Surgery+radiation therapy+hormone therapy | 2 y | Left breast |
| Edwards et al. (2017)7 | Vaginal squamous cell carcinoma | External radiotherapy and brachytherapy | 16 mo | Vulvar region |
Extragenital lichen sclerosus is generally asymptomatic, although it may present with associated dryness and pruritus. It most frequently affects the torso, neck, upper limbs, and flexor surface of the wrists. Lesions initially present as ivory-colored interfollicular polygonal papules that coalesce to form scleroatrophic plaques. Telangiectasia and follicular plugging may be observed in more advanced stages. Hemorrhagic blisters may appear owing to the fragility of the dermal-epidermal junction, as in our case.2
Diagnosis is essentially based on histologic findings, which show a specific pattern characterized by sclerosis or uniform hyalinization of the superficial dermis, and a lymphohistiocytic inflammatory infiltrate in an underlying band. Other more variable findings include thinning and atrophy of the epidermis, orthokeratotic hyperkeratosis, vacuolar degeneration of the basal layer, and dermal edema. Loss of elastic fibers is frequent in this disease.9
Genital lichen sclerosus only requires treatment in the event of associated pruritus or severe sclerosis. The most commonly used treatments are potent topical corticosteroids and topical calcineurin inhibitors. Systemic treatment is generally unnecessary in extragenital lichen sclerosus, as it is a benign skin disease that, unlike genital lichen sclerosus, presents a low risk of malignant transformation of the lesions.
We report a new case for the literature of lichen sclerosus induced by radiotherapy. Although only 4 reported cases of the disease exist in the literature, it is an entity we should be aware of given the current widespread use of radiotherapy.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Bonfill-Ortí M, Martínez-Molina L, Penín RM, Marcoval J. Liquen escleroso extragenital inducido por radioterapia. Actas Dermosifiliogr. 2019;110:69–71.