A 53-year-old female patient with Fitzpatrick phototype III was seen for asymptomatic nail lesions on the second and third fingers of the dominant (right) hand that had appeared 4–5 years earlier and had grown progressively (Fig. 1). She reported no personal or family history of melanoma or other skin cancers, had no concomitant diseases, and was not taking any medication. She did not perform any manual tasks that could result in trauma either in work or in her leisure time.
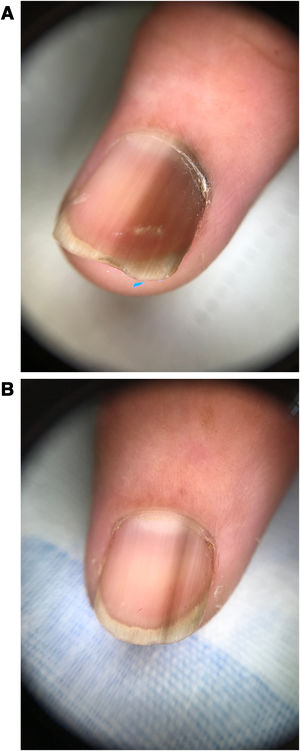
Physical examination revealed dark brown longitudinal striate melanonychia on the second and third fingers of the dominant (right) hand, consisting of narrow bands of homogeneous color and thickness. Hutchinson sign was absent. The remaining nails on the right hand, as well as those on the contralateral hand and the feet, were unaffected (Fig. 2A and B). No mucosal pigmentation was observed.
In evaluations performed 3 and 6 months later the lesions remained stable.
Nail matrix biopsy confirmed the absence of significant melanocytic proliferations.
When the patient was questioned further, the only relevant medical history was carpal tunnel-release surgery, which had been performed before the appearance of the nail lesions on the right hand and was repeated 2 years later due to recurrence. An electroneurogram revealed moderate focal sensory–motor neuropathy of the median nerve in the wrist. Currently, the patient is awaiting another intervention for the same reason.
Diagnosis and commentMelanonychia is the presence of melanin in the nail plate. If it acquires a linear morphology, from the proximal to the distal nail fold, it is known as longitudinal melanonychia. This melanin comes from melanocytes located in the nail matrix, most of which are in a quiescent inactive state. When activated, they can cause melanonychia through melanocytic activation or melanocytic hyperplasia.1
The causes of melanonychia due to melanocytic activation are multiple, and include physiological (race, pregnancy), regional (acute or repeated trauma, tight shoes, subungual foreign body, post-inflammatory hyperpigmentation, carpal tunnel syndrome), dermatological (psoriasis, lichen planus), systemic (Cushing syndrome, Addison syndrome), and iatrogenic (medication, radiotherapy, phototherapy) causes, as well as Laugier-Hunziker and Peutz-Jeghers syndromes.1–4 Causes of melanonychia due to melanocytic hyperplasia include lentigo, nevus, and melanoma.1
In general, traumatic melanonychia tends to affect the thumb and the second and third fingers of the dominant hand (used for clamping and grasping) and the first or fourth and fifth toes.1
Carpal tunnel syndrome is the main cause of acroparesthesia of the arms, which is bilateral in 50% of cases. It is more common in women aged 40–60 years. It is caused by compression of the median nerve in the tunnel formed by the carpal bones and the transverse carpal ligament. This nerve provides sensation and movement to the thumb and the index and middle fingers, as well as part of the ring finger. For this reason, the most common signs include tingling in the innervated areas, affecting mobility and sensitivity in advanced cases. The frequently unilateral skin manifestations of carpal tunnel syndrome include necrotic ulcerations and sclerodermiform changes (due to involvement of sensory and autonomic fibers). The following nail alterations have been described: hypertrophy of the cuticle, changes in coloration, Beau lines, subungual hyperkeratosis, onychomadesis, and one case of melanonychia of unknown origin. Cutaneous manifestations usually indicate serious involvement of the median nerve.5
In the present case, the fact that the melanonychia exhibited regular neat margins, affected several fingers, and remained stable over time was reassuring.2 In the absence of these factors a confirmatory biopsy would be necessary.
There are few published cases of longitudinal melanonychia in patients with carpal tunnel syndrome,6 which is considered an infrequent cause. The etiology of these nail alterations is unknown and is thought to be multifactorial. Microtrauma due to sensory denervation likely plays an important role. We present a case of melanonychia associated with advanced and operated carpal tunnel syndrome in a patient in whom we excluded other causes of longitudinal melanonychia. This is a rarely reported association.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García Castro R, Blanco Barrios S, González Pérez AM. Melanoniquia estriada y síndrome del túnel del carpo: una asociación escasamente reportada. Actas Dermosifiliogr. 2021;112:841–842.