Localized lipoatrophy is characterized by the loss of subcutaneous fat in a particular area of the body. In children, the condition is mainly related to subcutaneous or intramuscular injections of drugs or vaccines. Localized lipoatrophy is usually diagnosed clinically, although histopathologic examination can be necessary in some cases to rule out other causes such as connective tissue diseases and neoplasms.
We present the case of a healthy 8-year-old boy who was referred to our dermatology department for assessment of an asymptomatic lesion on his left thigh that had appeared 4 years earlier. A few weeks before the lesion appeared, the patient was diagnosed with streptococcal pharyngoamygdalitis and received treatment with an intramuscular injection of benzathine penicillin (600 000IU) on the lateral aspect of the left thigh. The lesion grew in proportion to the boy as he grew taller and gained weight. The boy had no personal or family history of autoimmune disease or history of trauma at the site of the lesion.
Physical examination revealed a 9×7cm depressed plaque of similar color to the adjacent skin on the anterolateral aspect of the left thigh. The lesion was covered with normal skin (Fig. 1). No similar lesions were detected at other sites. No loss of strength or sensitivity was observed in the lower left limb.
Blood tests were carried out, including complete blood count, kidney and liver function, cholesterol, triglycerides, lipase, complement, rheumatoid factor, antistreptolysin O, and antinuclear antibodies. No significant abnormalities were found. The patient tested negative for Borrelia burgdorferi.
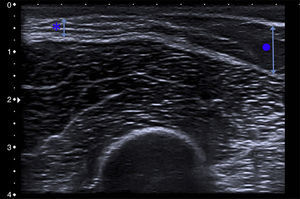
Ultrasound examination of the lesion revealed a complete loss of subcutaneous tissue alongside adjacent healthy skin. No muscular abnormalities were observed (Fig. 2). The parents declined to allow a biopsy of the lesion.
Treatment with medium-strength topical corticosteroids and topical calcineurin inhibitors was started. No improvement was seen after 2 months of treatment. The lesion has remained stable for 2 years of follow-up and no similar lesions have appeared at other sites.
Localized lipoatrophy can be classified as primary (or idiopathic) or as secondary to minor repetitive trauma injuries, injections of various drugs (penicillin, amikacin, methotrexate, corticosteroids, insulin)1–5 and vaccines,6 connective tissue diseases (lupus erythematosus, morphea, dermatomyositis), or malignant neoplasms.
Localized lipoatrophy secondary to drugs is characterized by the presence of depressed, asymptomatic lesions with a color and appearance similar to that of the adjacent skin. The lesions typically appear a few weeks or months after the injection and are usually located on the anterolateral aspect of the thighs, buttocks, or abdominal region.
The lesions tend to regress after a few months or years, although this depends on the drug involved and the degree of lipoatrophy. Lesions secondary to insulin injection tend to resolve spontaneously. Kumar et al.2 presented 2 cases of localized lipoatrophy caused by amikacin in which the lesions disappeared spontaneously after 2 and 3 months, respectively. Avilés-Izquierdo et al.4 reported a case associated with intramuscular corticosteroid injection in which the lesions regressed after 2 months. In the cases associated with methotrexate and penicillin that have been reported, the progression of the lesions is unknown due to lack of follow-up.1,3
In the case of our patient, the lesion remained stable after 2 years of follow-up. Haas et al.3 associated the persistence of the lesions in their patient with the possible existence of an underlying autoimmune disease. In the case of our patient, neither the clinical data nor the test results suggested the existence of an underlying autoimmune disease at any time during follow-up.
The etiology and pathogenesis of localized lipoatrophy are not clearly defined. The triggering mechanism is probably different for each drug. Insulin-induced lipoatrophy appears to be associated with local hyperproduction of tumor necrosis factor-α and interleukin-6, which would lead to a dedifferentiation of adipocytes.5 The injection itself could also play an important role in the development of lipoatrophy by causing macrophages to release cytokines, which in turn enhance the lipocyte catabolism and inhibit lipogenesis.6 In addition, hypoperfusion of the anterolateral aspect of the thigh due to anatomic variants of the lateral circumflex femoral artery would explain the lipoatrophy at that site.3 In the case of our patient, the injection of the drug, the anatomy and vascularization of the anterolateral aspect of the thigh, and the existence of ischemic phenomena caused by arterial trauma could explain the development of lipoatrophy.
The diagnosis of localized lipoatrophy is mainly clinical, although in some cases a skin biopsy can be necessary in order to rule out underlying disease. Histologic examination reveals a reduction in the size of the fat lobules of the hypodermis, with no evidence of fat necrosis, calcification, granulomas, or atypia. Cutaneous ultrasound can also be a useful tool in the diagnosis of patients with clinical suspicion of localized lipoatrophy. With cutaneous ultrasound, it is possible to quickly and safely observe—underneath a normal epidermis and dermis—a marked reduction in the subcutaneous tissue without the involvement of muscular tissue.
Because localized lipoatrophy tends to resolve spontaneously, many cases require no treatment. However, in cases in which the lesions persist, creating a significant cosmetic deficiency, some form of treatment may be indicated. Although no definitive treatment exists, intralesional corticosteroids have been used to treat lesions caused by insulin injections, with favorable results in some cases.7,8 This beneficial effect seems to be caused by the immunomodulating properties of the corticosteroids and to their capacity to induce the differentiation of adipocytes. However, because the reported cases are isolated, and because intralesional corticosteroid injections can themselves cause lipoatrophy, this treatment should be indicated with caution.
In corticosteroid-induced localized lipoatrophy, it has been shown that the intralesional administration of saline solution, autologous fat, or poly-L-lactic acid can have beneficial effects and improve the cosmetic appearance of the lesion.9,10
Avoiding injections in the anterolateral aspect of the thighs, rotating injection sites, and changing insulin pen needles are recommendations that can help patients and their family members prevent localized lipoatrophy secondary to drug injection.5
Please cite this article as: Vázquez-Osorio I, Rodríguez-Vidal A, Rosón E, Alonso-González J, Vázquez-Veiga H. Lipoatrofia localizada en un niño tras administración de penicilina intramuscular. Actas Dermosifiliogr. 2016;107:620–622.