Calciphylaxis or calcifying uremic arteriopathy is characterized by calcification of the media of the small arteries and arterioles of the skin, provoking cutaneous ischemia.1,2
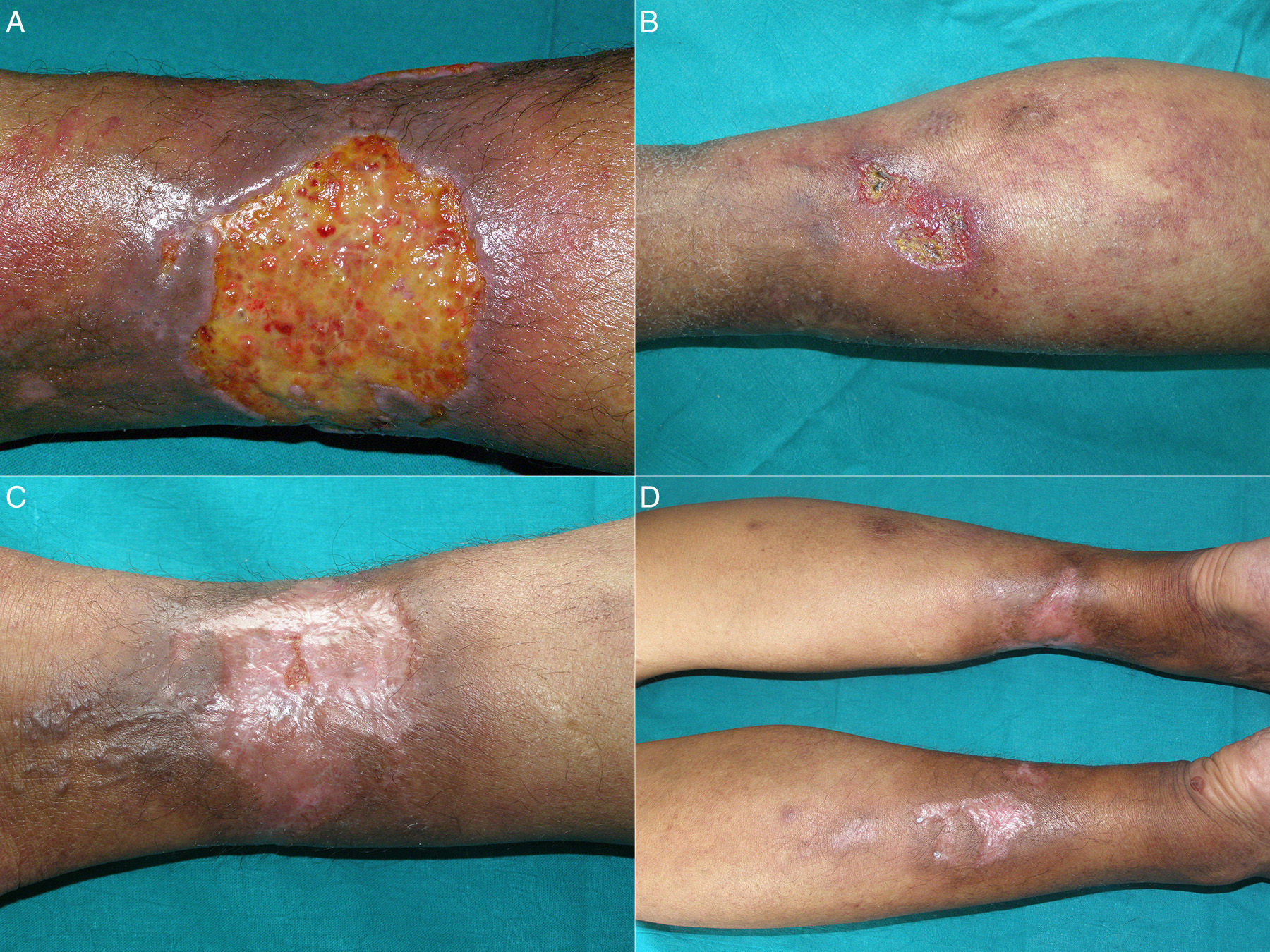
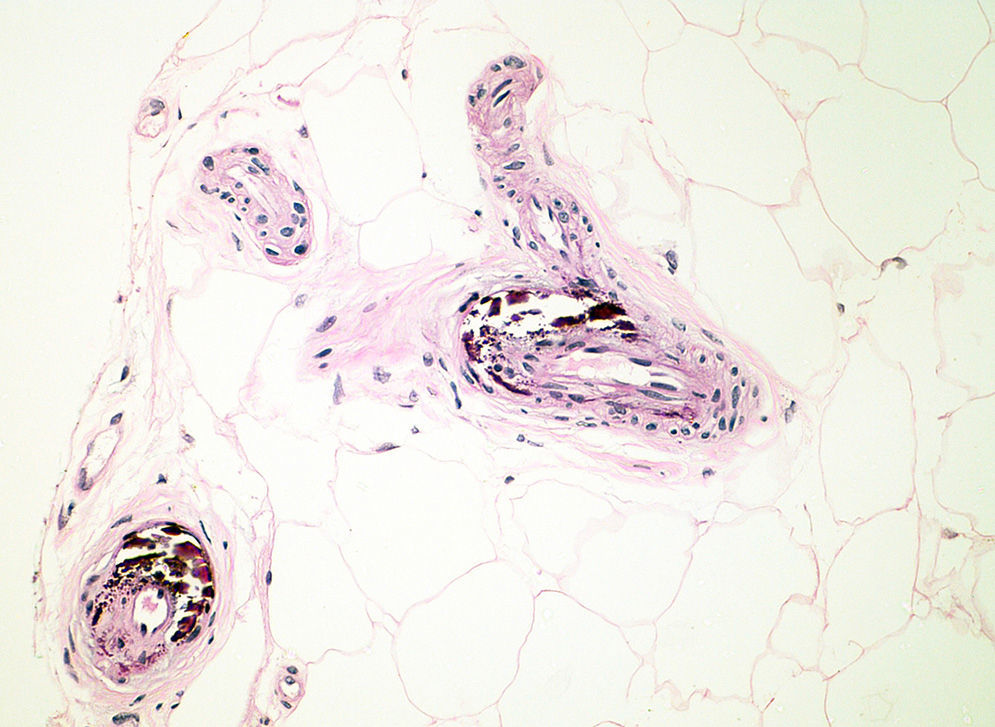
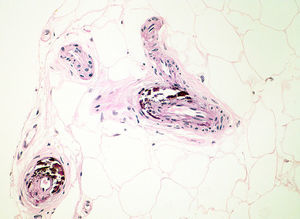
A 45-year-old woman with end-stage renal disease (ESRD) secondary to glomerulonephritis and on hemodialysis since 2008, consulted for a 10-month history of multiple, intensely painful ulcers on both lower limbs; the pain was resistant to opioids. She had previously undergone kidney transplant with subsequent rejection. Physical examination of the lower limbs revealed multiple skin ulcers, some with necrotic slough, on a background of livedo racemosa and retiform purpura. The largest ulcer measured approximately 6cm in diameter (Fig. 1, A and B). Important findings on the blood tests were secondary hyperparathyroidism with parathormone levels of 911pg/mL, calcium 10.1mg/dL (normal range, 8.2-10.3mg/dL), and phosphorus, 7.7mg/dL (normal range, 2.7-4.5mg/dL). Other additional tests, including complete blood count, general biochemistry, coagulation, serology for hepatitis B virus, hepatitis C virus, and human immunodeficiency virus, hypercoagulability study, autoimmunity, microbiology culture, and echocardiography were normal or negative. Skin biopsy was compatible with calciphylaxis (Fig. 2).
After signing the informed consent, the patient started off-label treatment with intralesional sodium thiosulfate 1/6molar, injecting 10mL of the solution around the borders of the ulcers. The only adverse effect was pain during the injection; this improved when oral transmucosal fentanyl was administered prior to the injections. After the first treatment, the patient reported rapid pain relief that enabled the opioids to be withdrawn. The treatment was repeated each month for 6 months, achieving complete remission of all the skin ulcers (Fig. 1C and D). Maintenance therapy was then administered with an intravenous sodium thiosulfate regimen after each hemodialysis session. At 6 months the patient returned to outpatients with new lesions. A further 3 monthly injections of sodium thiosulfate were therefore administered, and remission of the lesions was once again achieved. The patient now receives injections intermittently, whenever new symptoms develop, and overall control of the disease is good.
Calciphylaxis is characterized by the appearance of very painful skin ulcers and necrosis, mainly affecting patients with ESRD on hemodialysis, with an estimated prevalence between 1% and 4% in these patients.1–3 Mortality is high and is most commonly due to sepsis.4 Cases of ischemia of internal organs have been reported.2
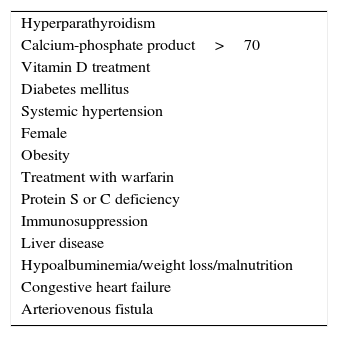
Risk factors for the onset of calciphylaxis in patients with ESRD are summarized in Table 1.1 Calciphylaxis has been described in patients without uremia. These cases are associated with primary hyperparathyroidism, malignancy, alcoholic liver disease, and connective tissue diseases, and are grouped under the name calcific nonuremic arteriolopathy.5
Risk Factors for the Onset of Calciphylaxis in Patients With End-Stage Renal Disease.
| Hyperparathyroidism |
| Calcium-phosphate product>70 |
| Vitamin D treatment |
| Diabetes mellitus |
| Systemic hypertension |
| Female |
| Obesity |
| Treatment with warfarin |
| Protein S or C deficiency |
| Immunosuppression |
| Liver disease |
| Hypoalbuminemia/weight loss/malnutrition |
| Congestive heart failure |
| Arteriovenous fistula |
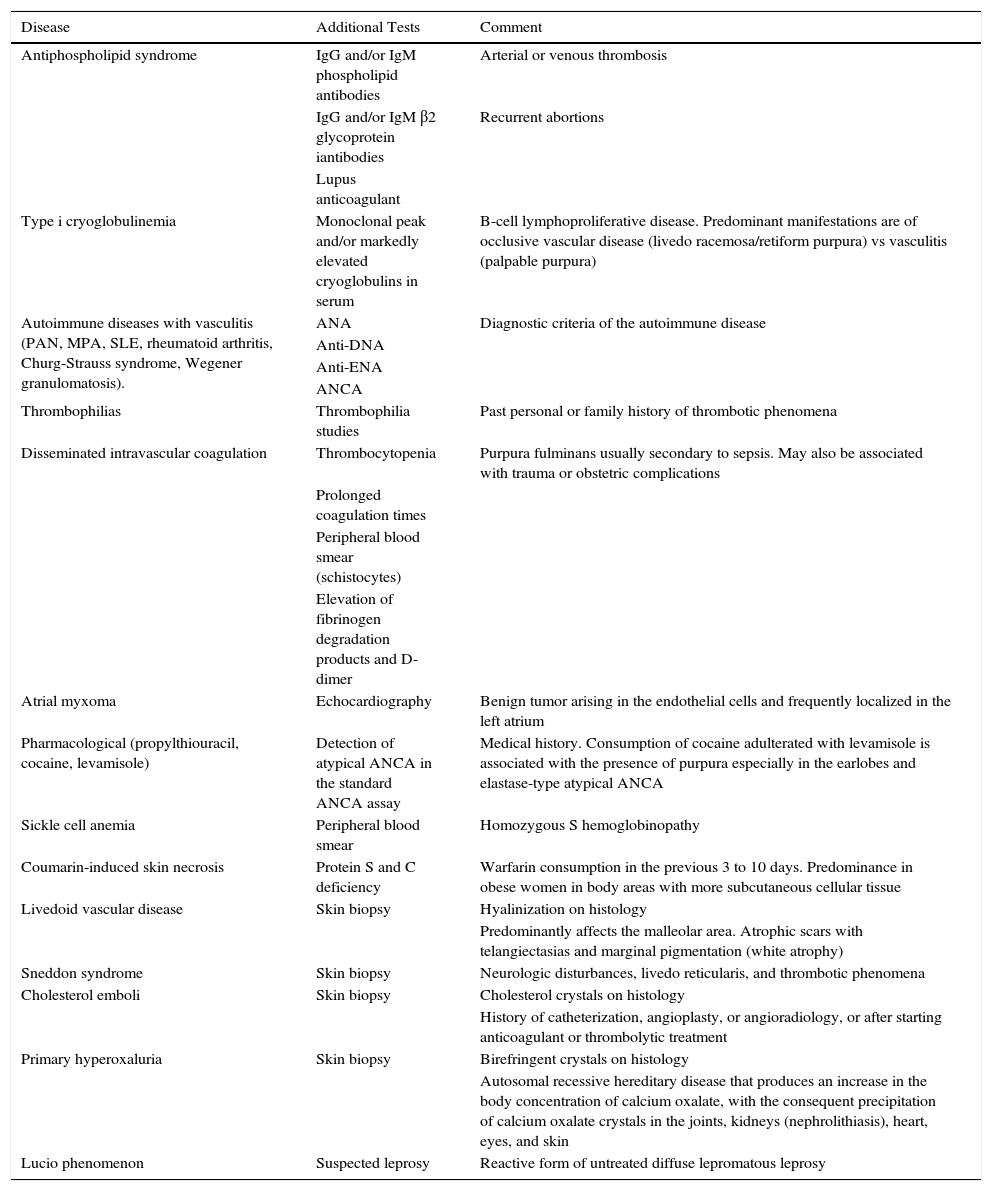
Clinically, calciphylaxis manifests as a livedo racemosa syndrome that progresses to retiform purpura and skin necrosis with the formation of very painful ulcers.6–8 In Table 2 we describe the differential diagnosis and workup of this syndrome.
Investigation and Differential Diagnosis of Patients With Suspected Calciphylaxis.
| Disease | Additional Tests | Comment |
|---|---|---|
| Antiphospholipid syndrome | IgG and/or IgM phospholipid antibodies | Arterial or venous thrombosis |
| IgG and/or IgM β2 glycoprotein iantibodies | Recurrent abortions | |
| Lupus anticoagulant | ||
| Type i cryoglobulinemia | Monoclonal peak and/or markedly elevated cryoglobulins in serum | B-cell lymphoproliferative disease. Predominant manifestations are of occlusive vascular disease (livedo racemosa/retiform purpura) vs vasculitis (palpable purpura) |
| Autoimmune diseases with vasculitis (PAN, MPA, SLE, rheumatoid arthritis, Churg-Strauss syndrome, Wegener granulomatosis). | ANA | Diagnostic criteria of the autoimmune disease |
| Anti-DNA | ||
| Anti-ENA | ||
| ANCA | ||
| Thrombophilias | Thrombophilia studies | Past personal or family history of thrombotic phenomena |
| Disseminated intravascular coagulation | Thrombocytopenia | Purpura fulminans usually secondary to sepsis. May also be associated with trauma or obstetric complications |
| Prolonged coagulation times | ||
| Peripheral blood smear (schistocytes) | ||
| Elevation of fibrinogen degradation products and D-dimer | ||
| Atrial myxoma | Echocardiography | Benign tumor arising in the endothelial cells and frequently localized in the left atrium |
| Pharmacological (propylthiouracil, cocaine, levamisole) | Detection of atypical ANCA in the standard ANCA assay | Medical history. Consumption of cocaine adulterated with levamisole is associated with the presence of purpura especially in the earlobes and elastase-type atypical ANCA |
| Sickle cell anemia | Peripheral blood smear | Homozygous S hemoglobinopathy |
| Coumarin-induced skin necrosis | Protein S and C deficiency | Warfarin consumption in the previous 3 to 10 days. Predominance in obese women in body areas with more subcutaneous cellular tissue |
| Livedoid vascular disease | Skin biopsy | Hyalinization on histology |
| Predominantly affects the malleolar area. Atrophic scars with telangiectasias and marginal pigmentation (white atrophy) | ||
| Sneddon syndrome | Skin biopsy | Neurologic disturbances, livedo reticularis, and thrombotic phenomena |
| Cholesterol emboli | Skin biopsy | Cholesterol crystals on histology |
| History of catheterization, angioplasty, or angioradiology, or after starting anticoagulant or thrombolytic treatment | ||
| Primary hyperoxaluria | Skin biopsy | Birefringent crystals on histology |
| Autosomal recessive hereditary disease that produces an increase in the body concentration of calcium oxalate, with the consequent precipitation of calcium oxalate crystals in the joints, kidneys (nephrolithiasis), heart, eyes, and skin | ||
| Lucio phenomenon | Suspected leprosy | Reactive form of untreated diffuse lepromatous leprosy |
Abbreviations: ANA, antinuclear antibodies; ANCA, antineutrophil cytoplasmic antibodies; ENA, extractable nuclear antigen; MPA, microscopic polyangiitis; PAN, polyarteritis nodosum; SLE, systemic lupus erythematosus.
Diagnosis is mainly clinical. Skin biopsy is the gold-standard test for the diagnosis of calciphylaxis, although systematically performing biopsies when this disease is suspected is not recommended because of the risk of infection or poor wound healing. Histopathology findings include calcification of the media of small arteries and arterioles, intimal proliferation, small-vessel thrombosis and endovascular fibrosis, necrosis of the subcutaneous cellular tissue, and panniculitis.2 No laboratory alterations specific to this disease have been detected. However, the presence of an elevated calcium-phosphate product increases the sensitivity for its detection.7
Among the imaging studies, ultrasound may show hyperechoic foci with a posterior acoustic shadow suggestive of calcifications. Modified mammography can facilitate early diagnosis of calciphylaxis. A bone scan can be useful to detect calcium deposits in the subcutaneous cellular tissue and thus help to define the extent of the disease and evaluate the response to treatment.9
Treatment protocols have not been standardized. Treatment is based mainly on the use of bisphosphonates and intravenous sodium thiosulfate. Sodium thiosulfate acts as an antioxidant and vasodilator, producing rapid pain relief, and as an intravascular and intraparenchymal chelator of calcium salts.3 Intravenous sodium thiosulfate is used at a dose of 25mg immediately after each hemodialysis session. This treatment is considered innocuous and is inexpensive. The most common side effects are nausea and vomiting, rhinorrhea, and headache. The most serious adverse effect is metabolic acidosis.10
In the scientific literature, only Strazzula et al.11 have described the use of intralesional sodium thiosulfate in 4 patients with calciphylaxis.
Although further studies are necessary to evaluate the therapeutic effect of intralesional sodium thiosulfate, we would like to draw attention to certain aspects. Intralesional treatment was very successful and led to rapid relief of the ischemic pain caused by calciphylaxis. In our patient, this intralesional treatment led to complete healing of the calciphylaxis-induced skin lesions, an objective not achieved with intravenous administration. We therefore consider that for cases that do not respond to standard intravenous treatment, the adjuvant role of intralesional sodium thiosulfate should be evaluated. The tolerance of the combined treatments was good, and although pain was the main limitation, it could be reduced by the previous administration of analgesia.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ossorio-García L, Jiménez-Gallo D, Arjona-Aguilera C, Linares-Barrios M. Calcifilaxis tratada con tiosulfato sódico intralesional. Actas Dermosifiliogr. 2016;107:360–363.