Diagnosis of melanocytic lesions is a complex process that mainly depends on the microscopic evaluation of biopsy samples. Multiple studies have shown low interobserver diagnostic agreement in such cases.1,2 These studies, however, have largely been small, non-randomized studies or studies that analyzed agreement between experts.
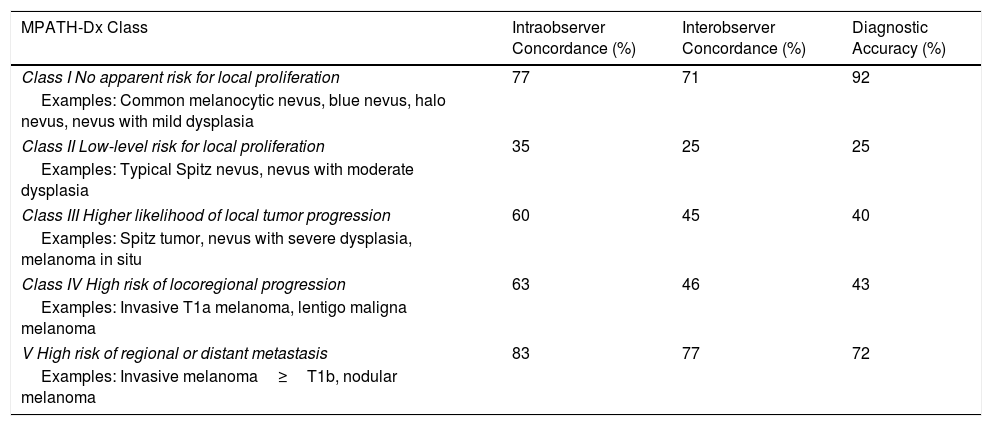
In a recent study, Elmore et al.3 published the results of the largest study to date to analyze diagnostic concordance in the setting of melanoma and melanocytic proliferations. They studied 187 US pathologists, most of whom (84%) had over 10 years’ experience analyzing melanocytic lesions and 42% of whom were considered an expert in the field. They selected 240 biopsy cases divided into groups of 48. A single hematoxylin-eosin–stained glass slide was available for each case. A reference diagnosis was established by 3 expert pathologists. Each of the participating pathologists was randomly assigned to a set of 48 cases and asked to diagnose them. The researchers grouped their responses using the Melanocytic Pathology Assessment Tool and Hierarchy for Diagnosis (MPATH-Dx) tool,4 which consists of 5 diagnostic classes ranging from low risk to high risk (classes i-v (Table 1). The same slides were re-evaluated at least 8 months later to check intraobserver concordance. The answers were compared with those given by the other pathologists in the group to evaluate interobserver concordance. These answers were then checked against the consensus reference diagnosis to evaluate observer accuracy.
Main Results from the Study by Elmore et al. (2017).
| MPATH-Dx Class | Intraobserver Concordance (%) | Interobserver Concordance (%) | Diagnostic Accuracy (%) |
|---|---|---|---|
| Class I No apparent risk for local proliferation | 77 | 71 | 92 |
| Examples: Common melanocytic nevus, blue nevus, halo nevus, nevus with mild dysplasia | |||
| Class II Low-level risk for local proliferation | 35 | 25 | 25 |
| Examples: Typical Spitz nevus, nevus with moderate dysplasia | |||
| Class III Higher likelihood of local tumor progression | 60 | 45 | 40 |
| Examples: Spitz tumor, nevus with severe dysplasia, melanoma in situ | |||
| Class IV High risk of locoregional progression | 63 | 46 | 43 |
| Examples: Invasive T1a melanoma, lentigo maligna melanoma | |||
| V High risk of regional or distant metastasis | 83 | 77 | 72 |
| Examples: Invasive melanoma≥T1b, nodular melanoma | |||
The results for intraobserver concordance varied according to lesion type. Concordance was highest for class i lesions (76.7%) and class v lesions (82.6%), but was considerably lower (35%-63%) for lesions in the intermediate classes. The results for interobserver concordance were similar (Table 1). Observer accuracy also varied significantly by lesion type and was 92% for class i lesions, 25% for class ii lesions, 40% for class iii lesions, 43% for class iv lesions, and 72% for class v lesions. Extrapolation of these results to the level of the population shows a diagnostic error rate of approximately 17.2% (8% for overinterpretation of lesion class and 9.2% for underinterpretation). They also show that based on the reference diagnosis, 16% of class iv or v lesions (invasive melanomas) would be classified as class i or ii lesions.
In brief, the study by Elmore et al.3 shows a low level of diagnostic concordance and accuracy for intermediate-class lesions such as dysplastic nevi, melanomas in situ, and invasive T1a melanomas that could result in over 17% of patients receiving incorrect treatments. Our study has several limitations, including the evaluation of a single glass slide, the nonuse of immunohistochemical staining and molecular assays, and the impossibility of asking for a second opinion. Without these limitations, the concordance and accuracy results may have been better. The results of our study, the largest of its type to date, indicate the need to improve current training systems and enhance the skills of specialists in the diagnosis and staging of melanocytic lesions. They also show the importance of using complementary diagnostic tools. Finally, the importance of adequate clinicopathologic correlation should not be overlooked.
Please cite this article as: Morgado-Carrasco D, Ertekin SS, Combalia A, Ferrandiz L. Diagnóstico histológico de lesiones melanocíticas y melanoma: todo un desafío. Actas Dermosifiliogr. 2018;109:825–826.