Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that is found predominantly in the flexures. The regions with a high density of apocrine glands (axillas, groin, buttocks, inframammary region, and perianal region) are those most often affected and the disease has a marked impact on the quality of life of patients. Though many therapeutic options are available, the response is inadequate in most cases and patients can present many years of recurrent outbreaks that have major physical and psychological sequelae.
For some years anti-tumor necrosis factor α (anti-TNF-α) agents have been a treatment option for patients with severe HS who do not respond to conventional therapy.1–4 Although there have been reports of cases of paradoxical psoriasis with anti-TNF-α agents,5–8 to our knowledge this disease has not yet been described in patients with HS treated with these drugs.
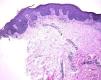
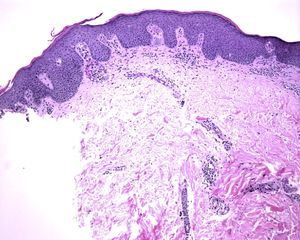
We report the case of a 50-year-old, obese, non-smoking woman with no relevant past history except for HS diagnosed at the age of 20 and that had worsened over the previous 3 years. She had received several treatments: daily antiseptic washes, topical clindamycin and mupirocin, several 6-month courses of minocycline 100mg per day, and a 3-month course of daily clindamycin 300mg plus rifampicin 300 mg. The response to all these treatments had been poor, so the patient was included in a clinical trial for treatment of HS with infliximab2 and began treatment at a dose of 5mg/kg every 8 weeks. The HS improved with the first infusion of the drug, but after 10 months of treatment the patient developed well-defined, scaly, erythematous lesions in the groin, axillas, and intergluteal and inframammary regions (Fig. 1). Direct microscopy with potassium hydroxide and culture were negative for fungi. Histology showed an epidermis with regular acanthosis, hyperkeratosis with parakeratosis, and suprapapillary thinning, confirming the diagnosis of flexural or inverted psoriasis (Fig. 2). At the time of writing, the patient was receiving intermittent treatment with topical hydrocortisone 2.5%, which enabled her to keep the psoriasis under control. She continued the treatment with infliximab and the clinical course of the HS was favourable.
The therapeutic management of HS is a challenge for the dermatologist. Several treatments have shown mixed results and none of them has been fully effective. Local treatments include antiseptic washes, topical antibiotics, and intralesional corticosteroid injections. Systemic treatments include oral retinoids, antibiotics such as minocycline or combined clindamycin and rifampicin, contraceptives alone or in combination with an antiandrogen, cycles of oral corticosteroids, and sulfone. Surgery, laser hair removal, photodynamic therapy, and even radiation therapy have also shown some efficacy.1
Recently, anti-TNF-α agents have shown good results in moderate to severe HS that is poorly controlled by conventional treatments.2–4 These drugs are used for inflammatory diseases in which TNF-α is involved, such as inflammatory bowel disease, rheumatoid arthritis, ankylosing spondylitis, and psoriasis. Inflammatory bowel disease has been associated with an increased risk of developing HS.9 Moreover, the risk of developing psoriasis is of 6% to 11% in patients with inflammatory bowel disease, a higher risk than in the general population.5,6 Smoking, treatment with lithium salts, and obesity are aggravating factors for both HS and psoriasis.1,9 In addition, TNF-α has been implicated in the pathophysiology of both diseases. Elevated levels of TNF-α, IL-10, and IL-1β have recently been reported in patients with HS, which would explain the good response to these drugs10; however, not all patients with HS respond to anti-TNF-α agents and most do so only partially.2–4 Furthermore, HS lesions are often superinfected by microorganisms and there is a theoretical risk of dissemination of the infection with anti-TNF-α agents.
Though anti-TNF-α agents are indicated for the treatment of moderate and severe forms of psoriasis, the possibility of paradoxical phenomena, such as the onset or exacerbation of psoriasis, is recognized with all of them (infliximab, etanercept, and adalimumab).5–8 Outbreaks of psoriasis associated with this drug usually appear as palmoplantar, pustular, or plaque-type psoriasis and more rarely as inverse psoriasis, as in our patient.6 The time of onset varies from 4 months to several years after the start of treatment.7,8 Depending on the severity of the psoriasis symptoms, the anti-TNF-α agent can be maintained or replaced by another immunosuppressant. In 85% of cases, the change to another anti-TNF-α agent does not solve the occurrence of psoriasis, which is therefore considered a class effect.8 The mechanism by which psoriasis occurs in patients treated with anti-TNF-α agents is unknown. It has been suggested that the decreased TNF-α causes an increase in interferon α, which in some patients leads to the development and worsening of psoriasis lesions, but further studies are needed to confirm this hypothesis.8,10 By contrast, interferon α levels are decreased in HS.10 This finding would explain the good response of HS to treatment with infliximab and the onset of psoriasis in our patient.
We stress the importance of this case because it is the first published case of the appearance of psoriasis in a patient with HS treated with an anti-TNF-α agent (infliximab), because it had an atypical presentation as flexural or inverse psoriasis, and because it showed a good response to treatment with only topical corticosteroids, without the need to interrupt the infliximab prescribed to treat the underlying disease.
Conflicts of InterestsDrs. Almudena González and Carlos Nuño-Ricotti declare that they have no conflicts of interest.
Dr. Luis Dehesa has participated in conferences for Abbott, Pfizer, and Astellas.
Dr. Francisco Kerdel has participated in conferences and studies for Amgen, Abbott, Jansen, Schering-Plough, Pfizer, and Eisai.
Please cite this article as: Nuño-González A, et al. Aparición de psoriasis flexural o invertida en una paciente con hidrosadenitis supurativa en tratamiento con infliximab. Actas Dermosifiliogr. 2012;103:936–7.