Dermatosis characterized by tissue eosinophilia arising in the context of hematologic disease is known as eosinophilic dermatosis of hematologic malignancy. The most commonly associated malignancy is chronic lymphocytic leukemia. Eosinophilic dermatosis of hematologic malignancy is a rare condition with a wide variety of clinical presentations, ranging from papules, erythematous nodules, or blisters that simulate arthropod bites, to the formation of true plaques of differing sizes. Histology reveals the presence of abundant eosinophils. We present 4 new cases seen in Hospital Arnau de Vilanova, Valencia, during the past 7 years. Three of these cases were associated with chronic lymphocytic leukemia and 1 with mycosis fungoides. It is important to recognize this dermatosis as it can indicate progression of the underlying disease, as was the case in 3 of our patients.
La dermatosis caracterizada por eosinofilia tisular que aparece en el contexto de un trastorno hematológico se conoce con el nombre de dermatosis eosinofílica asociada a proceso hematológico, siendo el más frecuente de todos la leucemia linfática crónica. Se trata de una entidad poco frecuente que tiene un amplio espectro morfológico, desde pápulas, nódulos eritematosos o ampollas que simulan picaduras de artrópodo hasta la formación de verdaderas placas de tamaño variable y en las que la histología se caracteriza por la presencia de abundantes eosinófilos. Presentamos 4 nuevos casos diagnosticados en nuestro hospital en los últimos 7 años, 3 de ellos asociados a una leucemia linfática crónica y un cuarto caso asociado a una micosis fungoide. La importancia de conocer esta dermatosis radica en el hecho de que puede indicar una progresión de la enfermedad de base, y así fue en 3 de nuestros pacientes.
We present the cases of 4 patients with hematologic neoplasms who developed lesions with clinical and histological features reminiscent of insect bites. All 4 patients were diagnosed with eosinophilic dermatosis (ED) of hematologic malignancy. In one of these patients, the underlying disease was a cutaneous T-cell lymphoma. This type of cutaneous eruption has previously been reported in patients with B-cell lymphomas, human immunodeficiency virus (HIV), congenital agammaglobulinemia, acute monocytic leukemia, and myelofibrosis.1–6
Case DescriptionsWe carried out a retrospective study of cases of ED of hematologic malignancy diagnosed in our hospital between 2009 and 2015. The clinical characteristics of the patients are summarized in Table 1. The patients were 1 woman and 3 men, aged between 53 and 86 years. Three of them were diagnosed with chronic lymphocytic leukemia (CLL) and one with mycosis fungoides (MF) CD3+, CD4–, CD7–, and CD8–. All 4 patients were referred for consultation by the Hematology Department because they had developed cutaneous lesions. The interval between diagnosis of the blood cancer and the appearance of the dermatosis varied from 2 months to 10 years. None of the 3 patients with CLL were receiving specific treatment for their hematologic disease at the time the skin lesions appeared: in case 1 because of sepsis caused by Klebsiella pneumoniae, which had led to the cessation of the third cycle of chemotherapy a few months earlier; in case 2 because the disease was in a very early stage; and in case 3 because the patient was in partial remission following 2 cycles of chemotherapy. The patient with MF had been receiving treatment with bexarotene for 2 months.
Clinical Characteristics of the Patients with Eosinophilic Dermatosis.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age, years | 69 | 86 | 71 | 53 |
| Sex | Woman | Man | Man | Man |
| Hematologic malignancy and stage | CLL IIB | CLL IA | CLL IB | MF IIA |
| Time elapsed since diagnosis of hematologic malignancy | 6 y | 7 y | 10 y | 2 mo |
| Treatment for hematologic disease | None | None | None | Bexarotene |
| Skin lesions | Papules | Plaques | Papules and plaques | Plaques |
| Site | Back/UL | Face/UL | Abdomen/UL/LL | Abdomen/LL |
| Treatment of ED | TC | TC | TC+OC | TC |
| Course of ED | Recurrent | Recurrent | Recurrent | Resolved |
| Course of hematologic disease | Death at 3 months | Progression to IB | Progression to IIB | No progression |
| Treatment of the hematologic disease after diagnosis of ED | Cyclophosphamide | Rituximab+chlorambucil | Ibrutinib | Continued on bexarotene |
Abbreviations: CLL, chronic lymphocytic leukemia; ED, eosinophilic dermatosis; LL, lower limbs; MF, mycosis fungoides; OC, oral corticosteroid; TC, topical corticosteroid; UL, upper limbs.
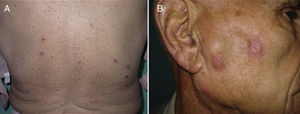
In all 4 cases, the presenting complaint was the appearance of a pruritic eruption with onset between 1 and 4 weeks earlier. Multiple palpable preauricular and cervical lymph nodes were found in Case 2 and accompanying B symptoms were observed in Case 3. The basic lesions varied:excoriated papules in Case 1 (Fig. 1A); erythematous papules in a linear pattern in case 2 (Fig. 1B); confluent papules of various sizes on the forearm in Case 3 (Fig. 2A); and poorly defined erythematous-violaceous plaques in patient 4 (Fig. 2B). The site most frequently affected was the upper limbs. In Case 1, ED developed when the patient was in hospital because of progression of her CLL. None of the patients reported any history of an insect bite.
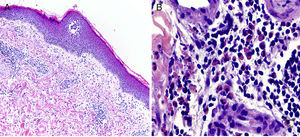
In all 4 cases, a histologic study was performed following staining with hematoxylin-eosin. Immunofluorescence was not performed since clinically the lesions were papules or plaques consistent with insect bites. In all 4 cases, histologic examination revealed a perivascular and periadnexal interstitial inflammatory infiltrate in the superficial and deep dermis composed of polymorphonuclear lymphocytes and abundant eosinophils (Fig. 3). The presence of malignant cells in the infiltrate was ruled out using fluorescence in-situ hybridization (FISH); no monoclonal rearrangement of lymphocytes was observed.
Patients 1, 2, and 4 were treated with topical corticosteroid therapy alone, with the addition of oral prednisone in patient 3. The lesions disappeared within a few weeks. In case 2, resolution coincided with the start of specific chemotherapy. The cutaneous lesions recurred in all of the patients with CLL over subsequent months. The patient in Case 1 died a few months after onset of the cutaneous symptoms and progression of CLL was observed in the other 2 patients after the diagnosis of ED. The patient with MF (Case 4) responded to topical corticosteroid therapy; ED was not associated with a worse prognosis and the patient is currently stable.
DiscussionThis clinical entity was first described by Weed in 1965.7 It was interpreted as an exaggerated hypersensitivity to mosquito bites in patients with CLL. It was never possible to demonstrate whether or not a bite was necessary to trigger the process and, after several nomenclatures in the intervening period, it is now known as ED of hematologic malignancy, a term that covers all the malignancies in which the condition has been described.1,8 We found 34 publications under the older term exaggerated reaction to insect bites, most relating to isolated cases. Table 2 shows the most recent cases published with the new nomenclature. This is a rare condition, primarily associated with CLL,1–5,7,8 although it has also been reported in association with other B-cell hematologic malignancies6,9–14 (mantle cell lymphoma, acute lymphoblastic leukemia, large cell lymphoma, multiple myeloma), and with acute monocytic leukemia, myelofibrosis, and nonmalignant processes, such as HIV infection and congenital agammaglobulinemia.3 Although the eruption usually appears several years after the diagnosis of the malignancy, cases have also been reported in which the condition developed before or at the same time as the malignancy.1
Comparison of Our Series With Cases Previously Reported in the Literature.
| Reference | Patients | Hematologic Disease | Type of Skin Lesion | Course and Treatment of ED | Course of Hematologic Disease |
|---|---|---|---|---|---|
| Martínez et al.8 (2006) | Man 69 y | CLL | Escoriated papules, vesicles, and blisters on back and limbs | Recurrent despite TC therapy | Progression |
| Hidalgo et al.4 (2010) | Man 80 y | CLL | Erythematous papules and nodules on limbs | Improvement with OC and antihistamine therapy | Progression |
| Farber et al.1 (2012) | Man 73 y | CLL | Erythematous papules and nodules on the face, trunk, and limbs | Resolved with CT. Recurrence treated with OC, doxycycline and antihistamines | Progression |
| Chassine et al.9 (2012) | 3 men 3 women 72-80 y | 3 CLL 2 mantle cell lymphomas 1 MALT lymphoma | Excoriated papules and plaques, vesicles and pustules on the face, trunk and limbs | P1, P2, P4-P6: Resolution with CT P3: spontaneous resolution | P1, P2, P6: no progression P3: diagnosis of blood disease and death at 2 months P4: progression and death at 18 months P5: diagnosis of blood disease |
| Two et al.6 (2014) | Man 50 y | Multiple myeloma | Blistering on limbs and trunk | Resolution with TC and CT | Progression |
| Penn et al.5 (2015) | Man 56 y | Diffuse large B-cell lymphoma | Erythematous papules and vesicles on limbs | Several recurrent outbreaks treated with TC, intralesional corticosteroids, and CT | Progression |
| Shin and Kim10 (2016) | Man 73 y | CLL | Cellulitis-like plaques on neck and blisters on limbs | OC. Several recurrences | No progression in relation to relapses (45 mo follow-up) Finally progression of the disease after 7 mo without relapse |
| Jayasekera et al.11 (2016) | Man 51 y | CLL | Papules, erythematous plaques, and vesicles on legs and dorsum of foot | Initial response to dapsone Started CT and OC | Progression |
| Our cases | 3 men 1 woman 53-86 y | 3 CLL 1 mycosis fungoides | Papules and plaques on the face, trunk and limbs | P1, P2 and P3: Relapses despite treatment with TC and OC P4: resolution after TC | P1: death at 3 months P2 and P3: progression P4: no progression (45 mo follow-up) |
Abbreviations: CLL, chronic lymphocytic leukemia; CT, chemotherapy; ED, eosinophilic dermatosis; MALT, mucosa-associated lymphoid tissue; MF, mycosis fungoides; OC, oral corticosteroid; P, patient; TC, topical corticosteroid
The pathogenesis of the condition is unknown, but it has been suggested that the leukemic cells may cause an imbalance in cytokines, which leads to increased interleukin (IL)-5 and ultimately to the proliferation of eosinophils. Other authors have suggested that the patient's underlying immunodeficiency followed by an immune stimulus (an insect bite, drugs, or a virus) may trigger an altered immune response with overexpression of IL-5.1,8
The clinical presentation takes the form of pruritic papules or hive-like nodules reminiscent of arthropod bites. Cases have also been reported involving true plaques of variable size and occasionally vesiculobullous lesions.1,3 Lesions usually affect exposed and unexposed areas of the skin and occur predominantly on the limbs. In many cases, the cutaneous symptoms recur in situations in which insect bites would be unlikely.
The characteristic histologic feature is the presence of an eosinophil-rich, perivascular and periadnexal, interstitial inflammatory lymphocytic infiltrate, which occasionally extends into the subcutaneous tissue.13 The lymphocytic infiltrate is predominantly composed of T cells (CD3+, CD43+, CD45RO+)1; when B cells are present they form polyclonal aggregates. No leukemic cells are observed.1,13 One case has been described in which FISH revealed the presence of malignant cells in the infiltrate of a biopsy from a patient with CLL.15 This did not occur in our patients.
In 2001, Byrd et al. proposed the set of diagnostic criteria shown in2Table 3.
Diagnostic Criteria for Eosinophilic Dermatosis of Hematologic Malignancy.
| Pruritic papules, nodules and/or vesiculobullous eruption refractory to standard treatment |
| Eosinophil-rich lymphohistiocytic infiltrate in the superficial and deep dermis |
| Exclusion of other causes of tissue eosinophilia |
| Prior or subsequent diagnosis of hematologic malignancy |
The differential diagnosis includes leukemia cutis, scabies, toxicoderma, hypersensitivity to insect bites, early stages of blistering diseases such as bullous pemphigoid and dermatitis herpetiformis, eosinophilic folliculitis, and Wells syndrome.1,8
To date, no relationship has been demonstrated between the onset of ED and the course of the underlying disease. However, a rapidly progressive course of CLL has been observed in some patients coinciding with the onset of ED.1–9,11 In our series, 3 of the 4 patients progressed to a more advanced stage of their hematologic disease, and 1 patient died due to CLL a few months after onset of ED. By contrast, in another recently reported case, a patient with CLL and recurrent ED remained stable for 45 months after initial onset of ED.10 Thus, the prognostic implications of ED in this setting are still unclear.
Many treatments have been proposed, but most are associated with partial response and frequent recurrence. Improvement has been achieved with specific chemotherapy.1,6 The condition is generally refractory to oral antihistamines and topical corticosteroids8 although in our patients the latter were the treatment of choice. The most effective and generally accepted treatment at the present time is oral corticosteroids at doses of 0.5-1 mg/kg/d.3 This regimen achieves good initial results, but relapse is common when the dose is reduced. UVB phototherapy would appear to be a good choice of therapy.2
We report 4 new cases of ED. Three were associated with CLL (the most common association reported in the literature) and the onset of ED was associated with a poor prognosis. The fourth case was associated with a cutaneous T-cell lymphoma, representing the first instance of this association reported in the literature. After 7 years of follow-up and treatment with oral bexarotene, the fourth patient has had no new outbreaks and remains stable. The cutaneous manifestation are ordinary lesions resembling insect bites. However, in the case of patients with a history of hematologic malignancy, the possibility of ED of hematologic malignancy should be considered and the patient should be closely monitored since, while the relationship is not entirely clear, the presence of ED may be an indication of progression of the underlying disease.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no private patient data are disclosed in this article.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lucas-Truyols S, Rodrigo-Nicolás B, Lloret-Ruiz C, Quecedo-Estébanez E. Dermatosis eosinofílicas asociadas a procesos hematológicos. Actas Dermosifiliogr. 2017;108:e39–e44.