Few epidemiological studies have investigated the incidence of allergic contact dermatitis in children. Underdiagnosis has been observed in some studies, with many cases in which the condition is not suspected clinically and patch tests are not performed. However, the prevalence of pediatric sensitization to allergens has been reported to be as high as 20%, and the diagnosis should therefore be contemplated as a possibility in this age group.
Material and methodsWe performed a retrospective analysis of the skin allergy database of the Dermatology Department of Consorcio Hospital General Universitario de Valencia. Children between 0 and 16 years of age diagnosed with allergic contact dermatitis in the previous 15 years (between 2000 and 2015) were included in the analysis. Epidemiological (age, sex, history of atopy) and clinical (site of the lesions, allergen series applied, positive reactions, and their relevance) variables were gathered.
ResultsPatch tests had been performed on 4,593 patients during the study period. Of these, 265 (6%) were children aged between 0 and 16 years. A positive reaction to at least one of the allergens tested was observed in 144 (54.3%) patients in that group. The allergens most frequently identified were the following (in decreasing order of frequency): thiomersal, cobalt chloride, colophony, paraphenylenediamine, potassium dichromate, mercury, and nickel. The sensitization was considered relevant in 177 (61.3%) cases.
ConclusionsMore than half of the children studied showed sensitization to 1 or more allergens, with a high percentage of relevant sensitizations. All children with a clinical suspicion of allergic contact dermatitis should be referred for patch testing. As no standardized test series have been developed for this age group, a high level of clinical suspicion and knowledge of the allergens most commonly involved are required when selecting the allergens to be tested.
Los estudios epidemiológicos sobre incidencia de dermatitis alérgica de contacto en población pediátrica son escasos. Algunos trabajos consideran que se trata de una entidad infradiagnosticada, y que en muchos casos no se sospecha clínicamente, no realizándose pruebas epicutáneas. No obstante se han comunicado tasas prevalencia de hasta el 20% de sensibilización a alérgenos en la población pediátrica, por lo que probablemente debería ser tenida en cuenta como una posibilidad diagnóstica en este grupo de edad.
Material y métodoSe ha realizado un análisis retrospectivo de la base de datos de alergia cutánea del servicio de Dermatología del Hospital General seleccionando los casos diagnosticados en niños de entre 0 y 16 años durante los u¿ltimos 15 años (año 2000 hasta 2015). El estudio incluye variables epidemiológicas (edad, sexo, antecedentes de atopia) y clínicas (localización de las lesiones, baterías de alérgenos empleadas, alérgenos positivos y su relevancia).
ResultadosDe los 4.593 pacientes estudiados con pruebas epicutáneas en los u¿ltimos 15 años, 265 (6%) correspondían a niños de 0-16 años. Ciento cuarenta y cuatro pacientes (54,3%) mostraron positividad para al menos uno de los alérgenos parcheados. Los alérgenos más frecuentemente identificados fueron en orden decreciente: tiomersal, cloruro de cobalto, colofonia, parafenilendiamina, dicromato potásico, mercurio y níquel. La sensibilización fue considerada de relevancia presente en 177 casos (61,3%).
ConclusiónMás de la mitad de los niños estudiados mostraron sensibilización a uno o más alérgenos, con un porcentaje importante de sensibilizaciones relevantes. Todo niño con sospecha clínica de dermatitis alérgica de contacto debería ser remitido para realización de pruebas epicutáneas. Al no existir pruebas estandarizadas en este colectivo se requiere un alto nivel de sospecha clínica y un conocimiento de los alérgenos más frecuentemente implicados de cara a seleccionar los alérgenos a parchar.
Allergic contact dermatitis (ACD) has traditionally been considered a disease of adults, and eczematous reactions in children are generally considered to be atopic. However, awareness of the importance of ACD in younger patients has been growing in recent years.1–3
Epidemiological studies of pediatric ACD reveal that the incidence of this disease is increasing.4–7 Nevertheless, the results of these studies are difficult to compare owing to differences in test methodologies, patch test allergens, demographics of the study population, and the selection criteria applied to the children referred for evaluation.
The objective of our study was to estimate the prevalence of ACD in children attending the skin allergy clinic of a tertiary hospital. We also sought to determine the most frequent allergens and the clinical and epidemiological characteristics of children with ACD.
Materials and MethodsWe identified all children aged 0 to 16 years referred to the skin allergy unit of our department for patch testing. In all cases, the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC) (Martitor) was applied, as were the patient's own products and additional series depending on the degree of clinical suspicion in each case. The allergens were applied to the apparently healthy skin of the patient's back and occluded for 48hours. Readings were taken at 48 and 96hours. The skin reaction was evaluated according to the criteria of the International Contact Dermatitis Research Group. All clinical data and the results of the readings were stored prospectively in a computerized database. The chi-square test was applied to compare percentages in the sensitized and nonsensitized populations. The Mann-Whitney test was used to compare age in the different groups.
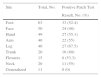
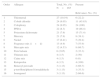
ResultsWe analyzed data from 4593 patients referred to the skin allergy clinic between the years 2000 and 2015. Of this total, 265 patients (5.7%) were children aged 0 to 16 years, and of these, 144 (54.3%) had positive results to at least 1 allergen (Table 1 and Fig. 1).
Epidemiological Characteristics of the Study Patients.
| Total | Positive Patch | Negative Patch | ||||
|---|---|---|---|---|---|---|
| (N=265) | Test Result (n=144) | Test Result (n=121) | ||||
| Sex, No. (%) | Boys, 110 (41.5) | Girls, 155 (58.5) | Boys, 59 (41) | Girls, 85 (59) | Boys, 51 (42.1) | Girls, 70 (57.9) |
| Age range, y | 1-16 | 2-16 | 1-16 | 2-16 | 2-16 | 2-16 |
| Age group, No. (%) | ||||||
| 0-2 y | 1 (0.4) | 0 (0) | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) |
| 2-5 y | 7 (2.6) | 7 (2.6) | 2 (1.4) | 3 (2.1) | 5 (4.1) | 4 (3.3) |
| 5-10 y | 30 (11.3) | 40 (15.1) | 16 (11.1) | 21 (14.6) | 14 (11.6) | 19 (15.7) |
| 10-15 y | 58 (21.9) | 85 (32.1) | 32 (22.2) | 44 (30.6) | 26 (21.5) | 41 (33.9) |
| >15 y | 14 (5.3) | 23 (8.7) | 8 (5.6) | 17 (11.8) | 6 (5) | 6 (5) |
Of the 144 sensitized children, 113 (84%) had positive patch test results with present relevance. A total of 302 patch test results were positive (mean of 2.1 positive results per patient).
The mean (SD) age of patients referred to the clinic was 11.1 (3.7) years. No significant differences in age were found between children with and without ACD.
As for distribution by sex, 155 of the 265 children were girls (58.5%) and 110 were boys (41.5%). The group of sensitized patients comprised 85 girls (59%) and 59 boys (41%); the group of nonsensitized patients comprised 70 girls (57.9%) and 51 boys (42.1%). The chi-square test revealed no significant association between sex and a positive patch test result.
No significant differences were found in the prevalence of sensitization with respect to age at onset (0-2 years, 2-5 years, 5-10 years, 10-15 years, and >15 years).
Positive reactions are shown by site in Table 2. The most commonly affected area was the trunk (16 positive results in 20 patients with lesions on the trunk [80%]).
Of the 265 children studied, 70 (26.4%) had a history of atopy. The prevalence of sensitization in children with no history of atopy was 1.3 times higher than in children with a history of atopy. The chi-square test revealed a slightly significant difference (P=.049) between the absence of a personal history of atopy and ACD.
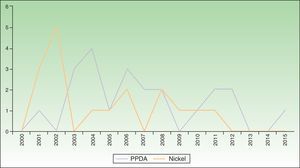
The most common allergens were, in descending order of frequency, thiomersal (27 cases), colophony (24 cases), paraphenylenediamine (PPDA, 22 cases), metals (potassium dichromate, 21 cases; mercury, 21 cases; and nickel, 17 cases), fragrances (mixes i and ii, 11 cases; Peru balsam, 6 cases), and rubber (mercapto mix, 12 cases; thiuram mix, 4 cases). The highest percentages of relevant cases were observed for colophony (100%), ketoprofen (100%), and PPDA (86.4%). The lowest percentages of relevant cases were observed for Peru balsam (33.3%), nickel (29.4%), and thiomersal (22.2%). Table 3 shows the most common allergens and cases with present relevance.
Most Common Allergens and Their Prevalence in the Pediatric Patients Studieda
| Order | Allergen | Total, No. (%) N=265 | Present |
|---|---|---|---|
| Relevance, No. (%) | |||
| 1 | Thiomersal | 27 (10.19) | 6 (22.2) |
| 2 | Cobalt chloride | 24 (9.05) | 11 (45.83) |
| 3 | Colophony | 24 (9.05) | 24 (100) |
| 4 | PPDA | 22 (8.3) | 19 (86.4) |
| 5 | Potassium dichromate | 21 (7.9) | 15 (71.4) |
| 7 | Mercury | 21 (7.9) | 8 (38.1) |
| 6 | Nickel | 17 (6.41) | 5 (29.4) |
| 8 | Fragrance mix (i+ii) | 13 (4.9) | 7 (53.9) |
| 9 | Mercapto mix | 12 (4.53) | 8 (66.7) |
| 10 | Peru balsam | 6 (2.65) | 2 (33.3) |
| 11 | Thiuram mix | 4 (1.5) | 2 (50) |
| 12 | Caine mix | 4 (1.5) | 0 (0) |
| 13 | Ketoprofen | 4 (1.5) | 4 (100) |
| 14 | Benzoyl peroxide | 3 (1.13) | 2 (66.7) |
| 15 | p-tert-Butylphenol formaldehyde | 3 (1.13) | 1 (33.3) |
| 16 | Isoeugenol | 3 (1.13) | 2 (66.6) |
Abbreviation: PPDA, paraphenylenediamine.
Thiomersal was the most common allergen, with 27 positive patch test results, although the relevance was unknown in most cases (87.8%).
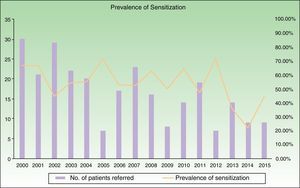
We found 17 cases of sensitization to nickel, with a prevalence of sensitization that was 6-fold higher in girls (P=.01). More than half of the children who were sensitized to nickel (58.8%) were cosensitized to cobalt. During the period 2010-2015, cases of sensitization to nickel decreased by 71% compared with 2004-2009. No cases of sensitization to nickel were diagnosed during the last 3 years of the study period (Fig. 2).
We recorded 22 cases of sensitization to PPDA, with a stable number of cases over time (Fig. 2). All the cases appeared after placement of a temporary black henna tattoo.
Of the 21 cases of sensitization to chrome, 15 (71.4%) involved the feet and were all associated with footwear and considered to be of present relevance.
Sensitization to mercury was considered to be of present relevance in 8 cases (38.1%). In 11 cases of sensitized children (52.3%), the patient was also sensitized to thiomersal.
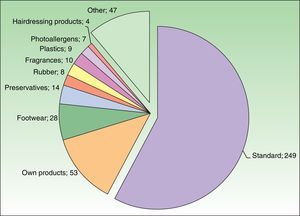
The most commonly used additional test series were footwear and preservatives (Fig. 3). Of the 302 positive patch test results, 262 (87%) were diagnosed using the standard series, and only 40 (13%) were confirmed allergens from additional series. The patient's own products were patch tested in 53 cases and confirmed the diagnosis in 17 cases; these would have gone undetected if the patient's own products (mainly sunscreens and topical drugs) had not been used in the patch test.
DiscussionWe found that the prevalence of sensitization in children referred to our skin allergy clinic was 54.3%, which is similar to data reported elsewhere.4–10 However, this parameter is very variable and depends on referral criteria, epidemiological characteristics, and exposure to allergens in the study population.
In contrast with our findings, many studies report a greater prevalence of ACD in females.6,7 Hormonal and exposure-related factors have been suggested, although most cases seem to be associated with more frequent wearing of jewelry and ear piercing at an early age in the case of nickel allergy. Although we did not find significant differences in the prevalence of sensitization between boys and girls, the prevalence of sensitization to nickel was 6-fold higher in girls, consistent with findings reported elsewhere. This could explain the female predominance of pediatric ACD found in many studies where nickel is the main cause of the condition.6,7
The association between atopy and ACD is controversial.1,2,6 In our study, we found a slightly statistically significant lower prevalence of ACD in atopic children. This result is consistent with the lower incidence of skin allergy in patients with atopy reported elsewhere.1,2,7
The most frequent allergens in our study were mercury compounds, metals present in jewelry, PPDA, products present in footwear, and fragrances. These allergens and their prevalence are very similar to those found in adults during the same period (Table 4).
Allergens Most Frequently Found in Adults During 2000-2015 and Their Prevalence.
| N=4328 | |
|---|---|
| Nickel | 979 (22.62%) |
| Cobalt chloride | 403 (9.31%) |
| Potassium dichromate | 314 (7.26%) |
| Paraphenylenediamine | 239 (5.52%) |
| Thiomersal | 236 (5.45%) |
| Kathon | 214 (4.94%) |
| Peru balsam | 195 (4.5%) |
| Fragrance mix | 182 (4.2%) |
| Mercury | 130 (3%) |
| Thiuram mix | 121 (2.78%) |
Mercury compounds were the most frequent group of allergens in the children we studied. In the case of thiomersal, the relevance of most reactions was unknown. This observation is consistent with those of other studies, where thiomersal was reported to be a very prevalent allergen in the general population, albeit with a low number of cases of relevant sensitization.1,7,8 Consequently, withdrawal of thiomersal from the standard series is currently being evaluated. Contact with broken mercury thermometers or use of antiseptics based on mercury compounds are additional routes of sensitization to mercury.
Jewelry and metals present in clothing and footwear were the second most common cause of sensitization after thiomersal. This observation is consistent with findings from many pediatric series, in which nickel was the most common allergen.7,11,12 Cosensitization to cobalt is common in patients sensitized to nickel or chrome.13,14 The number of cases of sensitization to nickel has fallen considerably since the implementation of European legislation on nickel content in jewelry.15
We detected a high number of positive reactions to PPDA, which is the third most frequent cause of ACD in our setting. As reported elsewhere, temporary black henna tattoos were the most frequent cause of sensitization.16 Use of PPDA in cosmetic products (with the exception of hair dyes) has been prohibited in the European Union since 2009.17,18 The number of cases of sensitization to PPDA fell during 2010-2015 compared with 2004-2009, although cases are still being reported despite the fact that its use in cosmetics is banned. Sensitization to PPDA is particularly important owing to the possibility of life-threatening severe acute reactions, potential long-term sequelae, and the ubiquitous presence of the allergen in many products in daily use, as well as its cross-reactivity with drugs from the para- group (eg, oral antidiabetic drugs, topical anesthetics, and sulfamides).19–21 Despite the health alert and legislative initiatives, more legal and educational measures are necessary if we are to regulate exposure of children to PPDA, specifically through temporary black henna tattoos.
Footwear is a common cause of ACD in children.22 The most frequent allergens in footwear-associated ACD in children are potassium dichromate (used to tan natural leather) and p-tert butylphenol formaldehyde (used as an adhesive).5,7,13 The European Commission regulation limiting the use of chrome salts in skin products that came into force on May 1, 2015 is expected to lead to a decrease in the frequency of chrome-induced ACD in the coming years.15,23
Colophony is a resin that is present in many adhesive health products. It is a major cause of iatrogenic ACD (Fig. 4), although there may also be cases of pediatric ACD caused by colophony in leather shoes, lipstick, and even musical instruments.24 Sensitization to colophony could be a marker of fragrance allergy.25 In the population we studied, all the cases of colophony allergy were associated with the use of adhesive dressings, thus confirming the major iatrogenic role of this substance.
Most cases of sensitization in our study were diagnosed using the standard series. The European Academy of Allergology and Clinical Immunology (EAACI) recently proposed a reduced standard series for children (Table 5).3 However, consistent with most epidemiological studies on pediatric ACD, we believe that the GEIDAC standard series is more useful when testing children, because the reduced series proposed by the EAACI does not include cobalt chloride, PPDA, potassium dichromate, mercury, or Peru balsam, all of which are among the 10 most frequent allergens in our study. Furthermore, the series does not include methylisothiazolinone alone, which is recommended based on increasing evidence from studies showing that the methylisothiazolinone/methylchloroisothiazolinone mix patch is insufficient.6,26
Series Recommended by the EAACI for the Study of ACD in Children.
| Allergens Recommended by the EAACI as the Standard Series in Children |
|---|
| Nickel sulfate: 5% pet |
| Thiuram mix: 1% pet |
| Mercapto mix: 1% pet |
| Mercaptobenzothiazole: 2% pet |
| Fragrance mix i: 8% pet |
| Fragrance mix ii: 14% pet |
| Colophony: 20% pet |
| Methylchloroisothiazolinone/Methylisothiazolinone: 100ppm aq |
| Sesquiterpene lactone mix: 0.1% pet |
Abbreviations: ACD, allergic contact dermatitis; EAACI European Academy of Allergy and Clinical Immunology.
The allergens that most frequently caused ACD in children in our study (see above) are classic allergens (thiomersal, metals, colophony) with well-recognized clinical manifestations. In the case of many of these allergens, various legislative measures have been put in place to limit the risk of sensitization, and this may explain the decreasing number of cases referred for evaluation in our study (Fig. 1). However, in recent years, there have been reports of emerging allergens whose growing importance lies in their ubiquity and frequency of sensitization, as well as in their poorer legal regulation.25–28 Such is the case of fragrances and preservatives in cosmetics.
Fragrances constitute a broad group of chemical compounds. Some studies place them as the second most common cause of contact allergy in adults in our setting, immediately after metals. These findings agree with our results in that fragrances were the fourth most common cause of ACD after thiomersal, metals, and PPDA. Patients with a positive result to fragrance markers in the standard series (fragrance mix i and ii, colophony, and Peru balsam) must undergo patch testing with a specific fragrance series in order to identify the individual fragrances the patient is sensitized to so that he/she can avoid them. It is important to remember that fragrances are present not only in perfumes and colognes, but also in a wide rage of products such as lipstick (Fig. 5) and makeup.
As for preservatives, methylchloroisothiazolinone and methylisothiazolinone are among the most frequent allergens in adult ACD in the most recent series.28 In our study, we found no cases of sensitization to methylchloroisothiazolinone and methylisothiazolinone in children. Nevertheless, these allergens are present in a wide rage of cosmetic products that are widely used in this age group (eg, gels, shampoos, wipes, and moisturizing creams).26,27 Some studies have shown a growing number of cases of allergy to methylchloroisothiazolinone and methylisothiazolinone in children and warn that in the future, these could be among the most common allergens in this population.26,27
Finally, with respect to legislation on allergens affecting children, regulation of cosmetic products for children is lacking, despite the strict regulation of allergens in children's toys.29 The year 2012 saw the publication of a resolution from the Council of Europe aimed at regulating cosmetic products for children aged under 3 years.30 However, the resolution is limited to general guidelines,31 without establishing which substances should be avoided in children, apart from those already banned in Directive 76/768/EEC17 and in Regulation EC 1223/2009.18 Thus, it is necessary to establish legislative measures to protect children—a particularly vulnerable group—from exposure to potential allergens that are currently in the cosmetic products usually aimed at this population.
In conclusion, ACD is a common condition in the pediatric population and must be taken into consideration when addressing a child with suggestive eczematous lesions and a compatible clinical history. Some classic allergens rarely lead to relevant sensitization or their incidence is decreasing. On the other hand, new allergens are emerging, especially in cosmetic products for children, which are often are poorly regulated. We should be alert to the presence of ACD due to emerging allergens that cause clinical manifestations that differ from those of “classic” allergens.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of dataThe authors declare that they have followed their institutional protocols on publication of patient data.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ortiz Salvador JM, Esteve Martínez A, Subiabre Ferrer D, Victoria Martínez AM, de la Cuadra Oyanguren J, Zaragoza Ninet V. Dermatitis alérgica de contacto pediátrica. Estudio clínico-epidemiológico en un hospital terciario. Actas Dermosifiliogr. 2017;108:571–578.