Myopericytomas are classified as benign pericytic (perivascular) soft-tissue tumors by the World Health Organization.1,2 Fewer than 200 cases of this rare tumor have been described in the literature, and fewer than 30 on the hands have been reported.
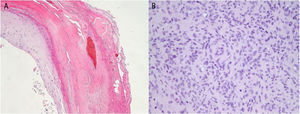
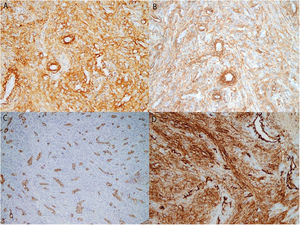
Our patient was a 48-year-old man with no relevant medical history who consulted us for a lesion that had appeared 9 months earlier on the pulp of the third finger of his right hand. He attributed it to an injury. Examination showed a hyperkeratotic lesion measuring 6×4mm in diameter (Fig. 1A). Under a dermoscope the lesion appeared pinkish-orange in color. Hemorrhagic areas and a well-defined collar were visible on the periphery (Fig. 1B). Pathology revealed a hyperkeratotic epidermis without atypia and with hemorrhagic areas in the stratum corneum (Fig. 2A). A proliferation of spindle cells in intersecting bundles surrounded thick-walled small-caliber vessels; no endothelial atypia was evident (Fig. 2B). The cells — especially those closest to vessels — were positive for actin and h-caldesmon; 10% stained positive for Ki-67 (Fig. 3).
The etiology of myopericytoma is unknown, but cases have been reported in association with injuries, compromised immunity, and Epstein-Barr virus infection.3,4
Myopericytomas usually present as well-defined nodules less than 2cm in diameter. They are slow-growing masses that are usually located on the upper extremities, head, or neck but may appear at any site.
The sensitivity of images obtained by magnetic resonance or ultrasound, for example, is low. Histology shows myopericytomas to be well-circumscribed, unencapsulated, and composed of oval myoid-appearing cells. Atypia and mitotic activity are absent. An eosinophilic or amphophilic cytoplasm usually surrounds the vessels. Immunohistochemistry detects positive staining for smooth-muscle actin and h-Caldesmon; findings are usually negative for desmin.2,5
Five histologic patterns have been described in myopericytoma, as follows, possibly corresponding to different stages of development: 1) a vascular pattern; 2) a glomus tumor-like pattern; 3) a nodular or cellular pattern, as in our case; 4) a multinodular or biphasic appearance; and 5) a piloleiomyoma-like pattern.2 Also described is a malignant variant with cellular pleomorphism, high mitotic activity and atypia, areas of necrosis, and an aggressive clinical course that can lead to metastasis and death.6
The differential diagnosis mainly considers the possibility of myofibromatosis, in which cells like those of myofibroblasts are found but grouped together and separated by collagen bundles. Glomus tumors must also be ruled out. These unencapsulated masses consist of nodules surrounded by connective tissue. Finally, angioleiomyomas must be considered. These tumors are usually well defined by a fibrous capsule of variable thickness consisting mainly of smooth muscle bundles lying among blood vessels in a fascicular pattern.7
We found a single reference for dermoscopic findings in myopericytoma. Mentioned were the presence of branching vessels on the surface.8 The hemorrhagic areas we observed under the dermoscope were related to extravasated blood cells in the dermis (Figs. 1 and 2). The unstructured orange-colored area corresponded to hemosiderin deposits. Tumor cells by themselves apparently do not give rise to a particular dermoscopic pattern. The clinical–dermoscopic differential diagnosis in our case would require consideration of other distal subungual lesions of the digits, such as subungual exostosis, which is characterized by areas of vascular ectasia, hyperkeratosis, onycholysis, and ulceration.9 Other such lesions are palmar–plantar warts, in which unstructured brownish-yellow and reddish-black globules corresponding to thrombosed vessels can be observed.10 These findings recall those we have described for this case of myopericytoma. Tungiasis may also present in a distal digital location, although the observation of a brownish circular area with a black dot in the center, which corresponds to the posterior part of the parasite's abdomen,11 makes this infestation difficult to confuse with a myopericytoma.
The recurrence rate after surgery, even when excision is incomplete, is less than 4%,6 and surgery is therefore the treatment of choice. Our case is consistent with this decision, given that no recurrence was observed after a year of follow-up even though the deep margin was still affected after excision.
In summary, in this new case of myopericytoma, a rare tumor associated with a history of trauma, the finger remained free of recurrence a year after incomplete excision. We have also described the dermoscopic appearance of the lesion. The only other reference to dermoscopic features we found in the literature differed from the ones we saw. More cases of myopericytoma should be reported and should include the appearance of these lesions under a dermoscope so that the characteristic patterns can be established.
Please cite this article as: Boix-Vilanova J, del Pozo Hernando LJ, Rodrigo Lara H, Corral-Magaña O. Miopericitoma digital distal: estudio dermatoscópico de un caso. Actas Dermosifiliogr. 2020;111:338–341.