To establish recommendations to determine, identify, and manage the psychological and emotional needs of patients with chronic inflammatory skin diseases in clinical practice.
MethodsA guided discussion was held at meeting of a nominal group of expert dermatologists and psychologists on the psychological and emotional needs of patients with chronic inflammatory skin diseases, how to manage these cases, and which referral criteria to employ. Based on the results of the discussion, and with the aid of a patient focus group and a review of the literature, a master document was drawn up with recommendations for discussion. A Delphi survey was circulated among a larger group of dermatologists and psychologists to assess the level of agreement with the recommendations.
ResultsTen recommendations were established and can be summarized as follows: explore the psychological sphere of the patients with open questions at the time of diagnosis and during the course of the disease; provide patients with clear explanations that address their concerns and inform them of the existence of patient associations; investigate symptoms of anxiety and depression and, if confirmed by means of a Hospital Anxiety and Depression score (HADS) of 11 or greater, consider referral to a mental-health specialist; and, during visits, create a climate of trust, empathize with patients, agree goals and treatment options with them, and motivate them to adhere to those treatments.
ConclusionsThese recommendations may help health care professionals address psychological and emotional aspects of their patients in daily clinical practice.
Establecer recomendaciones para conocer, identificar y manejar las necesidades psicológicas y emocionales de los pacientes con enfermedades inflamatorias crónicas dermatológicas en la práctica clínica habitual.
MétodosEn una reunión de grupo nominal con expertos dermatólogos y psicólogos, se realizó una discusión guiada sobre las necesidades psicológicas y emocionales de estos pacientes, cómo abordarlas, y cuáles serían los criterios de derivación apropiados. A partir de todo ello, con la ayuda de un grupo focal de pacientes y de una revisión de la literatura, se preparó un documento matriz con las recomendaciones para su discusión, así como una encuesta tipo Delphi para evaluar el grado de acuerdo con las mismas, que se hizo extensiva a más dermatólogos y psicólogos.
ResultadosSe establecieron 10 recomendaciones que podrían resumirse en las siguientes: explore la esfera psicológica de los pacientes con preguntas abiertas tanto en el momento del diagnóstico como durante el curso de la enfermedad. Dele explicaciones claras adaptadas a sus preocupaciones e infórmele de la existencia de asociaciones de pacientes. Explore si existen síntomas de ansiedad y depresión, y si se confirman mediantes una puntuación de 11 o más en la Hospital Anxiety and Depression Scale (HADS), valore una derivación a un especialista en salud mental. En las visitas, genere un clima de confianza, empatice con el paciente, consensúe con él los objetivos y opciones terapéuticas, y motívele para conseguir una buena adherencia.
ConclusionesEstas recomendaciones pueden servir a los profesionales sanitarios para que aborden de forma abierta y natural aspectos psicológicos y emocionales del paciente en la consulta diaria.
Chronic inflammatory skin diseases are very common in the general population. The estimated prevalence in Spain is as high as 2.3% for psoriasis1 and 3% for atopic dermatitis.2 The impact these conditions have on the lives of patients and their families is considerable.3,4
After the first symptoms appear, when the diagnosis is confirmed, and throughout the whole treatment period, these patients are frequently subject to stress, often accompanied by anxiety or depression. The prevalence of depression and anxiety can be as high as 30% in patients with psoriasis5–8 and ranges from 10% to 37% in atopic dermatitis.9 However, the patient's mood is not the only psychological repercussion of these conditions. Many patients with chronic inflammatory skin diseases report feeling stigmatized or isolated and present low self-esteem, negative emotions, and alexithymia.3,10–12
The prevalence of tobacco addiction and alcohol abuse has been reported to be even higher than 40% in patients with psoriasis.13 The findings in studies of patients with other chronic inflammatory skin diseases are very similar.14–16
These patients also experience other, equally serious, difficulties in their family life and workplace and in social interactions.17–23 In addition to causing the patient discomfort and disability and having a negative impact on those close to them, these diseases also lead to high consumption of social services and health care resources, thereby placing a considerable burden on the public health system.24
Despite all this evidence, clinicians in routine practice frequently fail to address the psychological and emotional aspects of these diseases as part of a comprehensive approach to their management, or do so inadequately due to a lack of training, guidelines, and recommendations.
In view of this situation, a decision was taken to produce a multidisciplinary consensus document with 3 main objectives: 1) to identify and understand the psychological and emotional needs of patients with chronic inflammatory skin diseases in routine daily practice from the time of diagnosis and throughout the course of the disease; 2) to explore how to approach these aspects of the disease during patient visits; and 3) to define criteria for referral to a mental health professional.
The overall aim was to encourage, facilitate, and improve communication with patients, shared decision making, investigation of psychological symptoms during patient visits, and referral of patients to mental health professionals when necessary. The authors of this document consider that any health professionals who treat patients with chronic inflammatory diseases—including dermatologists, nurses, primary care physicians, psychologists, and psychiatrists—could benefit from the application of these recommendations.
MethodsTo produce this consensus document, we used the nominal group technique and the Delphi method. The consensus statement was elaborated by distributing tasks and comments to the participants. These had been developed on the basis of a comprehensive review of the literature and the results of a patient focus group. The whole process was supervised by an expert methodologist.
The first step was to form a nominal group of 5 health professionals with recognized experience in caring for patients with chronic inflammatory skin diseases: 3 dermatologists and 2 psychologists. To identify the best candidates, a search was made for publications by Spanish professionals on the subject matter of this document on Medline and in the database of papers presented at the national congress of the Spanish Academy of Dermatology and Venereology (AEDV).
Nominal Group MeetingAt the initial meeting of this expert group, the first task was to define the scope, objectives, and target audience for the consensus document. Then, using a structured format, the group discussed all aspects of the psychological needs of patients with chronic inflammatory skin diseases, from the onset of symptoms and throughout the diagnostic process and the subsequent course of the disease. Individual patient characteristics, such as age and other circumstances, were taken into account. The group also considered the resources available to dermatologists and other professionals and what these professionals could do to make a positive contribution to the well-being of their patients. After this discussion, they defined the sections and tables that would make up the final document and decided to review the literature and conduct a patient focus group to explore different aspects of the psychological approach to these diseases.
Patient Focus GroupThe patient focus group included some patients belonging to patient organizations and others who did not. To recruit patients belonging to organizations, we contacted an organization and gave them a typological profile of the sample we needed for the focus group (representative in terms of age, gender, and disease severity). A sample group of patients who did not belong to any organization was recruited to complete the focus group. This was done by the methodological team using the same typological profile. A discussion map was created for the focus group. The areas covered were as follows: a) the psychological impact of the disease in general; b) the psychological impact in specific circumstances (at diagnosis, during a flare, in relation to the use of drugs, etc.); c) communication with those involved in their treatment; d) facilitators and barriers to communication; and e) aspects that could be improved.
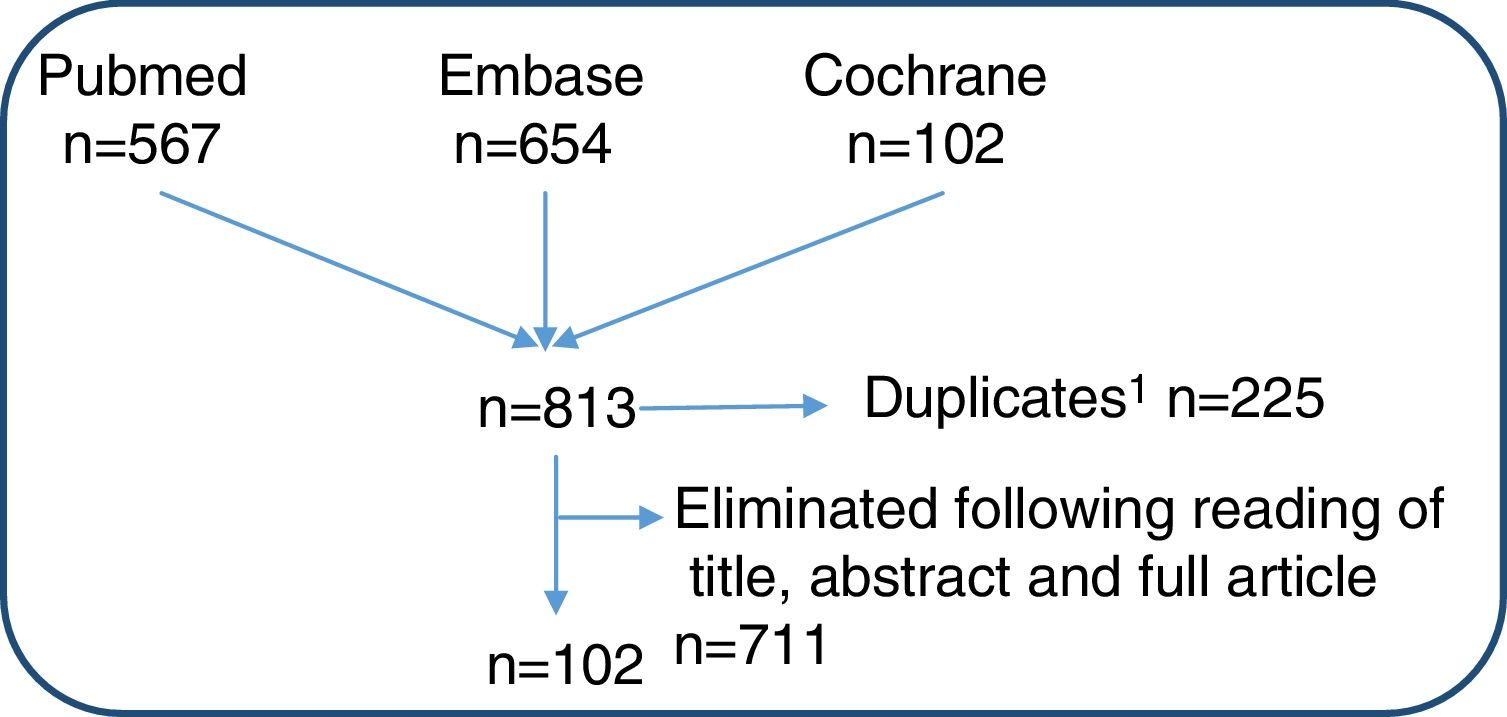
Literature ReviewAn extensive review of the literature was performed using predefined inclusion and exclusion criteria. The aim was to identify studies that included patients with psoriasis and other chronic inflammatory skin diseases and analyzed the prevalence and characteristics of psychological comorbidities and their impact on these patients. The search included meta-analyses, systematic reviews, clinical trials, and observational studies. We searched Medline, Embase, and the Cochrane Library from their respective start dates up to October 2017. Medical Subject Headings (MeSH) terms and free text terms were used to search all three databases and Pubmed Clinical Queries were also used in the case of Medline. The terms and queries used included the following: exp Psoriasis /, psoria*.tw., (pustulo* adj3 palm*).tw., ((chronic or plaque) adj3 psoriasis).ti,ab., ‘clinical trial’/exp, ‘randomized controlled trial’/exp, ‘crossover procedure’/exp, ‘behavior’/exp, ‘anxiety disorder’/exp, ‘stigma’/exp (Fig. 1).
DelphiA preliminary set of recommendations was developed on the basis of the information gathered in this way. After several rounds of revision by the group of experts, the proposed recommendations were submitted to an on-line Delphi vote. In the Delphi process, the expert group was enlarged to include a further 25 experts in this specific area (dermatologists, nurses, and psychologists) selected by the nominal group on the basis of their publications and activity as speakers on issues related to the psychological aspects of skin diseases. To select this panel, we searched Medline and the database of the AEDV's National Congress to identify Spanish professionals with publications on the subject matter of this document.
The Delphi participants rated each recommendation on a scale from 1 to 10 (1 = strongly disagree to 10 = strongly agree). Consensus was defined as a rating of 7 or higher from at least 80% of the panel. Recommendations that did not achieve this level of consensus were reassessed and, if necessary, redrafted and submitted to a second round of voting.
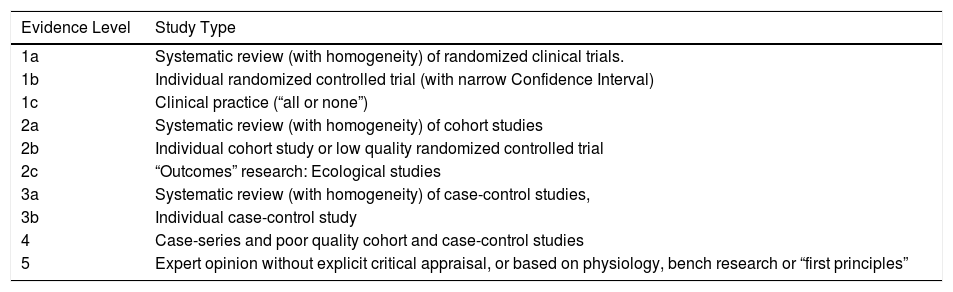
Final Consensus StatementAfter the literature reviews and the Delphi process, the final consensus statement was drafted. Each recommendation was assigned a level of evidence (LE) and a grade of recommendation (GR) using the Oxford Center for Evidence-Based Medicine methodology (Table 1).25 The level of agreement (LA) was determined as described above. The definitive consensus document was then reviewed by the experts, who added the final comments.
Levels of Evidence and Grades of Recommendation Defined by the Centre for Evidence-Based Medicine at the University of Oxford.
| Evidence Level | Study Type |
|---|---|
| 1a | Systematic review (with homogeneity) of randomized clinical trials. |
| 1b | Individual randomized controlled trial (with narrow Confidence Interval) |
| 1c | Clinical practice (“all or none”) |
| 2a | Systematic review (with homogeneity) of cohort studies |
| 2b | Individual cohort study or low quality randomized controlled trial |
| 2c | “Outcomes” research: Ecological studies |
| 3a | Systematic review (with homogeneity) of case-control studies, |
| 3b | Individual case-control study |
| 4 | Case-series and poor quality cohort and case-control studies |
| 5 | Expert opinion without explicit critical appraisal, or based on physiology, bench research or “first principles” |
| Grade of Recommendation | |
|---|---|
| A | Consistent level 1 studies |
| B | Consistent level 2 or 3 studies or extrapolations from level 1 studies |
| C | Level 4 studies or extrapolations from level 2 or 3 studies |
| D | Level 5 evidence or troublingly inconsistent or inconclusive studies of any level |
Source: Oxford Centre for Evidence-Based Medicine25
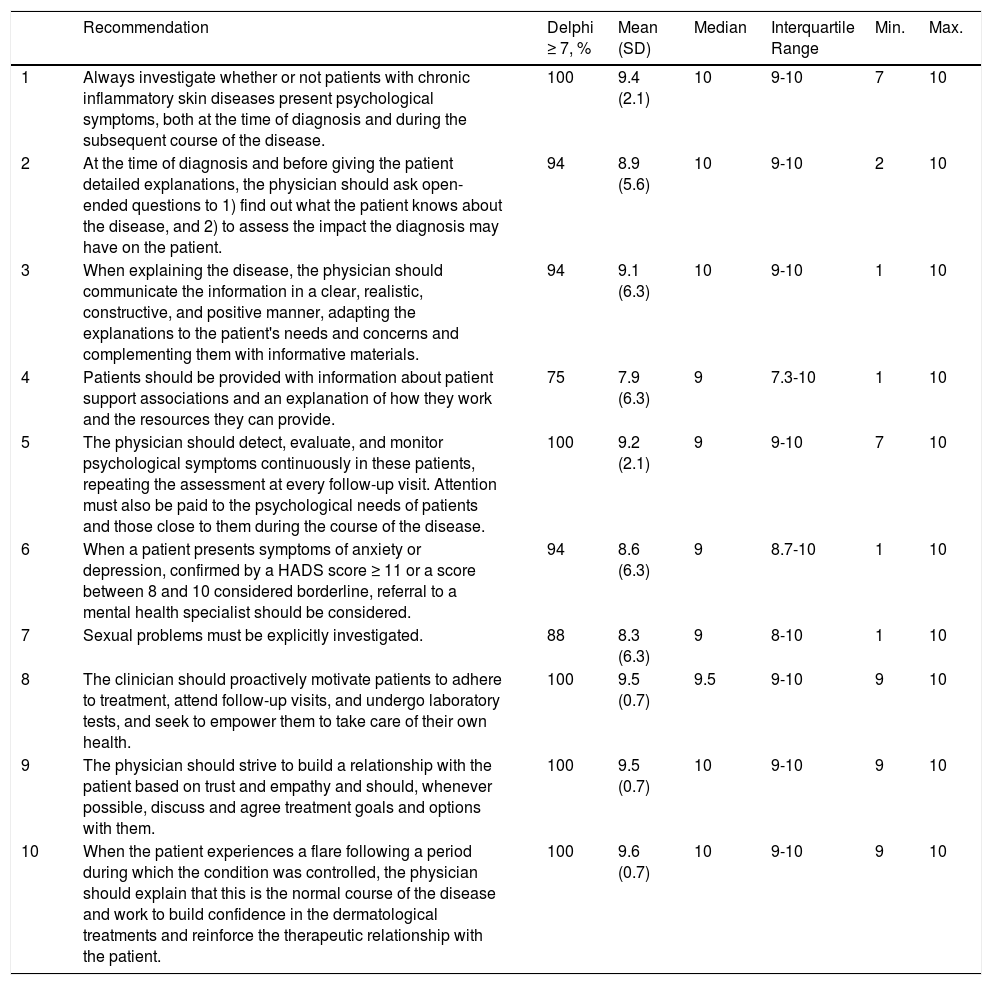
The recommendations of this consensus statement and the results of the Delphi process (60% response rates) are shown in Table 2. As well as explaining and justifying each recommendation throughout the document, we have also provided examples in italics to illustrate how each recommendation can be put into practice. It should be noted that, while the recommendations refer to all chronic inflammatory skin diseases, much of the evidence came from studies in patients with psoriasis, which we consider to be the paradigm for these disorders.
Delphi Results for the Recommendations on the Psychological Needs of Patients with Chronic Inflammatory Skin Diseases.
| Recommendation | Delphi ≥ 7, % | Mean (SD) | Median | Interquartile Range | Min. | Max. | |
|---|---|---|---|---|---|---|---|
| 1 | Always investigate whether or not patients with chronic inflammatory skin diseases present psychological symptoms, both at the time of diagnosis and during the subsequent course of the disease. | 100 | 9.4 (2.1) | 10 | 9-10 | 7 | 10 |
| 2 | At the time of diagnosis and before giving the patient detailed explanations, the physician should ask open-ended questions to 1) find out what the patient knows about the disease, and 2) to assess the impact the diagnosis may have on the patient. | 94 | 8.9 (5.6) | 10 | 9-10 | 2 | 10 |
| 3 | When explaining the disease, the physician should communicate the information in a clear, realistic, constructive, and positive manner, adapting the explanations to the patient's needs and concerns and complementing them with informative materials. | 94 | 9.1 (6.3) | 10 | 9-10 | 1 | 10 |
| 4 | Patients should be provided with information about patient support associations and an explanation of how they work and the resources they can provide. | 75 | 7.9 (6.3) | 9 | 7.3-10 | 1 | 10 |
| 5 | The physician should detect, evaluate, and monitor psychological symptoms continuously in these patients, repeating the assessment at every follow-up visit. Attention must also be paid to the psychological needs of patients and those close to them during the course of the disease. | 100 | 9.2 (2.1) | 9 | 9-10 | 7 | 10 |
| 6 | When a patient presents symptoms of anxiety or depression, confirmed by a HADS score ≥ 11 or a score between 8 and 10 considered borderline, referral to a mental health specialist should be considered. | 94 | 8.6 (6.3) | 9 | 8.7-10 | 1 | 10 |
| 7 | Sexual problems must be explicitly investigated. | 88 | 8.3 (6.3) | 9 | 8-10 | 1 | 10 |
| 8 | The clinician should proactively motivate patients to adhere to treatment, attend follow-up visits, and undergo laboratory tests, and seek to empower them to take care of their own health. | 100 | 9.5 (0.7) | 9.5 | 9-10 | 9 | 10 |
| 9 | The physician should strive to build a relationship with the patient based on trust and empathy and should, whenever possible, discuss and agree treatment goals and options with them. | 100 | 9.5 (0.7) | 10 | 9-10 | 9 | 10 |
| 10 | When the patient experiences a flare following a period during which the condition was controlled, the physician should explain that this is the normal course of the disease and work to build confidence in the dermatological treatments and reinforce the therapeutic relationship with the patient. | 100 | 9.6 (0.7) | 10 | 9-10 | 9 | 10 |
Abbreviations: HADS, Hospital Anxiety and Depression Scale; Max, maximum; Min, minimum.
The treatment objectives defined in the existing guidelines and consensus statements on chronic inflammatory skin diseases are mainly expressed in terms of objective disease-related clinical variables, such as the Psoriasis Area Severity Index (PASI) in the case of psoriasis and the Eczema Area and Severity Index (EASI) in the case of atopic dermatitis.26 While variables that assess the patient's subjective experience, such as quality of life, are gradually being introduced, these assessments are very often inadequate. In addition, it has been reported that even patients whose psoriasis is well-controlled with treatment may have emotional and social needs that are not being addressed.27,28 To address this problem, the biopsychosocial model, currently recommended for the treatment of any chronic disease, calls on clinicians to detect and treat patients’ psychological problems rather than focusing exclusively on their physical symptoms, because there is evidence that management of psychological symptoms, providing the patient with appropriate information, and effective communication enhance the doctor-patient relationship and improve the prognosis.29–32
In this document, we will describe the areas that should be addressed and how to explore the patient's affective symptoms using a method based mainly on the use of open-ended questions and questionnaires.
Recommendation 1Always investigate whether or not patients with chronic inflammatory skin diseases present psychological symptoms, both at the time of diagnosis and during the subsequent course of the disease (LE, 5; GR, D; LA, 100%).
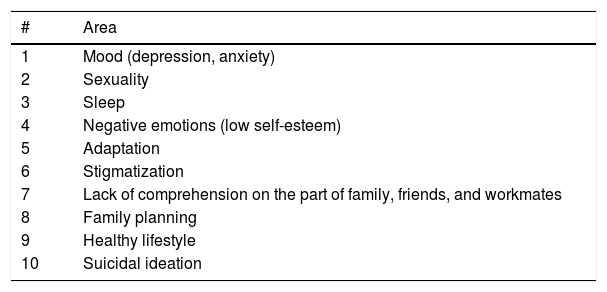
Many authors have suggested that psychological symptoms develop during the course of these diseases, but it has been shown that a high percentage of patients with palmoplantar pustulosis or psoriasis already present anxiety on diagnosis.33 It should be borne in mind that certain psychological variables—mood (depression, anxiety), personality traits, and the level of social support the patient receives—play a key role in the way these patients cope and the course of the disease.32 For this reason, the panel recommends that clinicians should be aware that psychological problems may be present from the onset of the disease (Table 3).
Areas That Should Be Considered When Assessing the Psychological Needs of Patients with Chronic Inflammatory Skin Diseases.
| # | Area |
|---|---|
| 1 | Mood (depression, anxiety) |
| 2 | Sexuality |
| 3 | Sleep |
| 4 | Negative emotions (low self-esteem) |
| 5 | Adaptation |
| 6 | Stigmatization |
| 7 | Lack of comprehension on the part of family, friends, and workmates |
| 8 | Family planning |
| 9 | Healthy lifestyle |
| 10 | Suicidal ideation |
Diagnosis can have a considerable emotional and psychological impact on patients. Moreover, they tend to come to the visit with preconceived ideas (gleaned through internet searches and from talking to those around them) and these preconceptions may give rise to fear, anxiety, or uncertainty.
Therefore, the first objective with respect to the patient's psychological needs at this time is to forge a therapeutic alliance.
A desirable aim by the end of the first visit is to have reassured the patient and communicated optimism while delivering a realistic message about their disease and helping them to cope effectively with this new chronic condition.
The way a patient perceives the disease and deals with it is influenced by the way the diagnosis is disclosed and depends on the message communicated by their physician.34 It has been shown that effective communication can prevent the development of psychological symptoms—including anxiety, depression, and distress—and has a positive influence in other important areas, such as adherence to treatment.29,35 Effective communication involves (among other things): 1) finding out what the patient already knows and adapting the message to what he or she wants or is prepared to understand at the time, progressing gradually if necessary; 2) a clear, objective, and realistic treatment plan, which is discussed and developed with the patient so that they will see it as their own plan and not something that has been imposed on them; and 3) giving the patient space to vent emotions (that is, letting them express their emotions and listening actively). It can make a very positive contribution to the management of the chronic condition if the patient perceives that the attending dermatologist and the medical services in general are accessible: for example, open channels of communication with patients (easy access to visits, contact with nursing staff, telephone and email contact, etc.).
Recommendation 2When informing the patient about the diagnosis, and before giving detailed explanations, the physician should ask open-ended questions to find out what the patient knows about the disease and to assess the impact the diagnosis may have on them (LE, 5; GR, D; LA, 94%).
Phrases like the following can be useful in this context:Before we go into details, may I ask what you already know about atopic dermatitis? Has your GP talked to you about psoriasis or maybe you have talked to a friend or family member about it? The results indicate that your condition is probably rosacea. Have you ever heard of rosacea? What do you know about this disease? Where did you get this information? The patient's answers to these questions will provide information about their level of stress during the visit and the likely impact of the confirmed diagnosis. Taking their answers into account, we can adapt the message and our explanations to reduce stress, address false beliefs, clarify the patient's preconceived ideas, and so on.
The next step is to find out what are the patient's main concerns in this new situation so that we can focus (at least a large part of our information) on these at a later stage. We can approach the subject as follows: From what you’ve heard about psoriasis, is there anything in particular that bothers you? What are you most worried about? Have you noticed changes at home or at work since you developed the disease? The patient's family situation and workplace are also areas of interest.
Since, particularly at the outset, the patient will not have developed a close relationship of trust with their doctor and/or may need to talk about intimate issues, we can also ask open questions or make comments and then leave the door open for them to respond when they are ready to do so without feeling pressured. For example: This skin condition can sometimes make people feel really uncomfortable in their daily life. If at any time you feel that way, let's talk about it. We can work on that together.
If there is time, you can ask patients about their family situation: talk to them about their relationships with their partner, parents, children, etc. If they work, you can ask about their work environment: how much they interact with colleagues (at meetings, for example), whether their work involves requirements in terms of physical image, what the repercussions might be if they had to request sick leave, etc. Several studies have reported a very high incidence of problems in these areas.4,18,36,37 Another area that should be explored is the patient's social support network (whether they are socially active or isolated, and so on). If time is limited at the first visit, these areas can be explored further during subsequent visits.
Recommendation 3When explaining the disease, the physician should communicate the information in a clear, realistic, constructive, and positive manner, adapting the explanations to the patient's needs and concerns and complementing them with informative materials (LE, 5; GR, D; LA, 94%).
Recommendation 4Patients should be provided with information about patient support associations and an explanation of how they work and the resources they can provide (LE, 5; GR, D; LA, 75%).
To reduce the psychological impact of our explanation or description of aspects of the disease, we can use phrases like the following: We know what you have and we are going to help you to deal with this condition.
Particularly during the initial visit, and even throughout the first few visits, it is unlikely that the patient will be able to fully absorb or understand all the explanations and messages they receive. For this reason, information should be imparted gradually, starting with the points the patient is most concerned about. All of the information provided should be adapted to what the patient needs and wants to know and can understand at the time. Other ways of educating patients include written materials, such as leaflets, and advice on recommended websites. It can be very useful to provide written as well as oral information, especially in the case of individuals with certain profiles, such as people who live alone. The panel also recommends that patients should be informed about relevant patient support associations because these organizations have many informative resources especially designed to help patients.38
When talking to patients, we should avoid, whenever possible, the use of technical medical terminology. The following are the kinds of words and expressions that can have a negative impact on patients: You have a chronic disease.You will experience recurrent flares.This condition develops because your immune system has gone crazy and is attacking your body. These can be replaced by other expressions, as follows: This is a long-term disease. Your blood levels of certain inflammatory substances are high, but we are continuously learning more about this process, and this new knowledge has led to new and better treatments. In short, whatever the message, we should try to empathize with the patient when delivering it.
It is also very important to validate the patient's feelings and concerns. If we want to connect with a patient, it is important to listen carefully to what they say and then acknowledge the statement verbally: I understand that you are worried about the side effects of the medication, but we can get these to improve a great deal and we are going to be monitoring the treatment continually to make sure that you are healthy and feel well. Patients who have a good relationship with their physician tend to play a more active role in managing their disease and to attend regular check-ups. They also trust us because they feel we understand them, and this trust favors adherence to the treatment regimen.
Another goal during this phase is to forge a strong therapeutic alliance with the patient by gaining their trust and making sure that they feel understood. Phrases like the following could help to develop this bond: I am going to be helping you for a while and we will be working together to treat this condition;I understand your situation and we will be seeing each other again. I am sure you will have more questions and doubts, but don´t worry we will solve them.
Follow-UpOver time, with additional visits, most patients become less anxious about their condition. Even so, it is important to check whether they have acquired a good understanding of their diagnosis and of the treatment plan.
We should also take advantage of follow-up visits to continue to assess the patient's psychological needs. Some affective symptoms may even occur after the skin condition has improved: in psoriasis, for example, the psychological impact on the patient persists even after the skin lesions have cleared.27 It is very important, therefore, to assess the possible involvement of organs and systems other than the skin.
Recommendation 5The physician should detect, evaluate, and monitor psychological symptoms continuously in these patients, repeating the assessment at every follow-up visit. Attention must also be paid to the psychological needs of patients and those close to them during the course of the disease (LE, 5; GR, D; LA, 100%).
For this reason we should continue to ask open questions using phases like the following: Is there anything you have stopped doing because of the skin condition? If you ever want to we can talk about ....It is possible that because you have this disease you are feeling X, or you are experiencingY. If that happens, you can tell me and we can talk about it.
On the other hand, take advantage of follow-up visits to continue analyzing which aspects of their condition most worry or bother the patient. With this knowledge, we can tailor the treatment regimen as well as the information and explanations we give them. It has been reported that one of the symptoms that most bothers patients with psoriasis and atopic dermatitis is itch, followed by (to a lesser extent) fatigue and pain.39 As in the diagnostic phase, we can ask open-ended questions. For example, when one of these symptoms is present, we can make specific mention of it: As well as curing the skin lesions, this treatment will also reduce the itch.
Since many patients associate stress with exacerbation of their skin condition,40 we can address this issue indirectly to discover what circumstances the patient associates with flares and advise them to avoid these in the future. Similarly, we can investigate which coping strategies tend to improve their condition and reinforce these. For example: Can you think of anything that might have brought on this flare?It seems that when you delegate household jobs everything goes better. That seems to me to be a very wise decision. This may be a good time to recommend relaxation techniques and physical exercise, explaining the benefits of these activities and how they may improve the condition.41
Since many chronic inflammatory skin diseases go through cycles made up of of flares followed by periods of remission, we must explain this characteristic in the most positive manner possible, emphasizing the many treatment options that are available. Regular follow-up visits facilitate early detection of flares and patients should also be offered the possibility of an unscheduled visit if this should be necessary. The lesions may reappear, but don't worry, we will be ready to treat them promptly.
Unlike at the time of diagnosis, when patients are often blocked, during follow-up they will have doubts and need more information. Visit preparation is a strategy that can help in this respect. Tell patients to write down their doubts when they occur to them and bring theire notes with them to the next follow-up visit. We can also take advantage of moments during a visit, when for example we have to write up something on the computer, to talk to the patient about their concerns: While I am writing up your medical history, take a moment to think a little about whether you have any questions about the disease, the treatment or anything else or whether there is anything else you wanted to talk about at this visit.
On the other hand, also with a view to building the patient's trust and improving their adherence to treatment and to their appointment schedule, we can use the same strategies as those described for use at the time of diagnosis: Always remember at every visit that I am here to help you.Our job is to help you with any doubts or problems you may haveand make sure you are well informed about the medical services you can turn to when you are not feeling well. We can also use the time to show the patient that, in addition to all the purely medical care, there are other resources, such as patient support associations.38
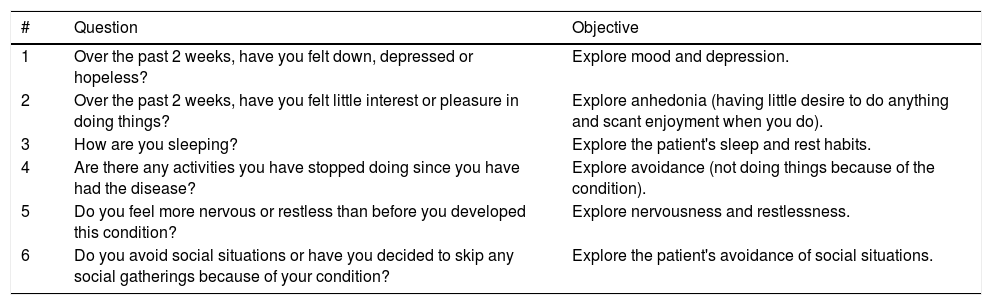
Since the time allocated to each patient visit is usually short, it can be very helpful to use targeted questionnaires, such as the Dermatology Quality of Life Index (DLQI), the Hospital Anxiety and Depression Scale (HADS), Goldberg's Anxiety And Depression Scale (GADS), and Skindex. The DLQI can be used to encourage patients to express their feelings, providing us with information about what areas we need to explore further. However, it does not assess everything that should be addressed in relation to the patient's emotional and psychological well-being. To complete the assessment we can use the HADS42 or the GADS43 questionnaires. If an emotional problem is detected, referral to a mental health specialist should be considered. In such cases, we recommend the HADS questionnaire because it is the tool that has been used most in dermatology. It can be helpful to use a few questions (3-4) to screen for the most important psychological symptoms that must be evaluated (Table 4).
Screening Questions Relating to the Most Important Psychological Symptoms for Consideration in Patients with Chronic Inflammatory Skin Diseases.
| # | Question | Objective |
|---|---|---|
| 1 | Over the past 2 weeks, have you felt down, depressed or hopeless? | Explore mood and depression. |
| 2 | Over the past 2 weeks, have you felt little interest or pleasure in doing things? | Explore anhedonia (having little desire to do anything and scant enjoyment when you do). |
| 3 | How are you sleeping? | Explore the patient's sleep and rest habits. |
| 4 | Are there any activities you have stopped doing since you have had the disease? | Explore avoidance (not doing things because of the condition). |
| 5 | Do you feel more nervous or restless than before you developed this condition? | Explore nervousness and restlessness. |
| 6 | Do you avoid social situations or have you decided to skip any social gatherings because of your condition? | Explore the patient's avoidance of social situations. |
Finally, during this phase, the panel also recommends continuing to maintain a generally positive, constructive, and empathetic attitude in all communications with the patient.
In the following section, we describe a series of psychological disorders frequently observed in these patients, which should be taken into account during follow-up. When such problems are detected, it is also important to check whether they are due to the skin condition or to other causes.
Recommendation 6When a patient presents symptoms of anxiety and depression, confirmed by a HADS score of 11 or higher or a score between 8 and 10 considered borderline, referral to a mental health specialist should be considered (LE, 5; GR, D; LA, 94%).
It is important to discuss the referral with the patient and jointly agree on the final decision, explaining that the additional care will make it easier to manage the disease.
Depression and anxiety. In patients with psoriasis, for example, it is thought that the prevalence of depressive symptoms or clinical depression during the course of the disease can be as high as 30%.5–8 In many cases, however, the symptoms of anxiety or depression may not be serious, and an empathetic attitude may be enough to gradually bring the affective symptoms under control. The HADS questionnaire42 can be used to assess the patient's affective state and referral to a mental health specialist should be considered if the emotional problem is confirmed. The patient's use of antidepressant or anxiolytic drugs should also be investigated.
Stigmatization. It is very common for patients with chronic inflammatory skin diseases to feel stigmatized.3,10–12 Stigmatization is defined as a situation in which an individual, due to their condition, is relegated to a social category rejected by the rest of society. In psoriasis, stigmatization—primarily caused by feelings of rejection, guilt and shame—has been correlated with itch intensity, stress prior to exacerbation, depressive symptoms, and quality of life.10
As well as detecting cases of stigmatization, we should also evaluate the patient's perception because they may misread or magnify the problem. The following are some ways of doing this: Have you ever felt rejected? Think about that question, and we will talk about it later. Sometimes a patient anticipates rejection, which in the event does not occur. In such cases, we can also propose alternatives: I understand your concern. Let's work on that and see what we can do to make sure you can go to the party and feel comfortable. Positive coping strategies should also be reinforced: Often, if you are able to talk about your condition openly and explain it to others, you will feel better and the people around you will get used to it. For example, talk to people at your gym and workplace and tell them that you have psoriasis. Different strategies will be needed depending on the individual characteristics of each patient. Finally, this can be a good opportunity to further empower the patient: These are strategies that will help to reduce your stress. I know that you don't want to do that, but I am sure you can. Let's work on this together.
Lack of understanding from family, friends, and in the workplace. Many patients feel that they are not understood by those around them. We must keep 2 things in mind in this situation: the first is that this perception of incomprehension can contribute negatively to the patient's condition and well-being; and the second is that the success of treatment also depends, in part, on the patient having good family and social support. Consequently, we must investigate the situation and take action if necessary, as we did with stigmatization: Do your family members, friends, and co-workers know that you have psoriasis? Do you think they understand what is happening to you?
If the patient is not understood or feels misunderstood, our first task is to gain a better understanding of their environment and the scope of the problem. Unless the case is particularly complex, we can encourage the patient to explain the disease to those around them and to be patient. It may help if they understand that these conditions are generally not well understood by the public. Making the situation natural can be very helpful: As part of your treatment, I encourage you to lead as normal a life as you can. You should try to meet up with your family and friends as usual. If you like going out to parties and having fun, then do that. And if there is something you used to do and now feel you cannot do, we can talk about that and think about it. I am sure we can find lots of other activities you will be comfortable with and can enjoy.
Sleep Disorders. Sleep disturbance is common in this group of patients.22,44,45 In psoriasis and atopic dermatitis, sleeping problems may be exacerbated by comorbid conditions or symptoms, including obstructive apnea, restless legs syndrome, painful and itchy skin lesions, and joint pain.22,44
Exploring this problem can also help us to detect others, such as depression and anxiety, which can be associated. We can assess the problem in the ways described above and in this case we can also provide information, for example: It is very normal for you to have trouble sleeping. Providing the patient with sleep guidelines and sleep hygiene strategies may be advisable.
Substance addiction. The prevalence of smoking in patients with psoriasis has been reported to reach 40% and even higher. Some studies have shown that the intensity and duration of addiction correlates with the severity of the skin disease.13,46–48 A high prevalence of smoking has also been observed in patients with other chronic inflammatory skin, diseases.14–16 The same occurs with alcohol abuse.49–51 Patients sometimes adopt maladaptive coping strategies—such as drinking alcohol—to deal with social situations, to escape from their problems, or to avoid facing up to their situation. These habits also favor systemic inflammation and associated physical and mental comorbidities, additional reasons for screening for these behaviors.52,53 It is important to refer patients with such addictions for appropriate treatment.
Recommendation 7Sexual problems must be explicitly investigated (LE, 5; GR, D; LA, 88%).
Sexual and reproductive health. The results of several studies have confirmed the high prevalence and marked impact of these inflammatory diseases on sexual function.54,55 Some of the risk factors associated with sexual dysfunction are disease severity, genital lesions, female sex, age, and joint involvment.54,56 When the dysfunction is severe, referral to an appropriate specialist is recommended.
Given that sexual matters are a very sensitive and intimate area for many people, we can explore this topic using open-ended questions and/or explanations, such as the following: As I mentioned before, this disease may affect your sexual relationships. If you ever have any questions about that or want to talk about it, please just ask. The DLQI contains a direct question on the topic of sexual problems and can help us to explore this area further with the patient.
The panel also recommends talking to all patients, men as well as women of childbearing age, about their desire to have children. This is essential if we are to recommend appropriate family planning measures and clarify the patient's doubts about the genetic component of the diseases.
Recommendation 8The clinician should proactively motivate patients to adhere to treatment, attend follow-up visits, and undergo laboratory tests, and seek to empower them to take care of their own health (LE, 2b; GR, B-C; LA, 100%).
The panel considers patient motivation to be fundamental. We must ensure that patients are committed, involved and truly convinced of the need to take their medication or apply topical treatments and feel that they are worth it. They must understand the need for treatment and feel that the treatment plan is their own and not something imposed on them by the dermatologist. Techniques such as the motivational interview can help us to achieve these goals.
This is a key point. Many patients with chronic inflammatory skin diseases do not adhere to the treatment plan. While this is particularly true in the case of topical treatments,57 a lack of adherence to systemic regimens has also been reported.58 We may encounter patients affected by factors that do not favor adherence, such as older patients, people who live alone, and patients with a low educational level or who hold certain cultural beliefs.
During follow-up, it may be necessary to change the pharmacological regimen. The change of treatment may be due to lack of efficacy. In such cases, the patient may be frustrated and/or anxious. If the change is due to an adverse event, the patient may experience feelings of loss or fear. In both cases, it is very important to reinforce the messages conveyed previously: Don’t panic, this is something that happens, but we have other drugs to treat your condition. Just because thishappened with this drug does not mean the same thing will happen with another. We will continue to monitor your case closely.
Finally, in relation to therapy and adherence to the regimen, the panel recommends that professionals should never reprimand patients and should avoid paternalistic attitudes.
Recommendation 9The physician should strive to build a relationship with the patient based on trust and empathy and should, whenever possible, discuss and agree treatment goals and options with them (LE, 5; GR, D; LA, 100%).
We must also adapt the treatment to the patient's needs. In line with current guidelines, therapeutic decisions and goals must be shared.35,59 Furthermore, it has been shown that good physician-patient interaction and communication favors adherence.30 In this respect, it is important to bear in mind 2 important aspects of the patient's point of view. The first is their needs and expectations in terms of what they are looking for or think they can achieve; the second is the management of any doubts and fears they may have regarding the safety of the drugs they will be taking.
First we must explore the patient's goals: what he or she hopes to achieve with the treatment. During this process, we can also help them to adjust their expectations, which may be too ambitious or not ambitious enough. If we manage to get the patient to make the goals their own, it will be easier for them to adhere to the prescribed treatment regimen. We can ask them questions like the following: What would you like to achieve with the treatment of your illness? What do you think we can achieve?
The panel also considers it important that patients understand that there are many therapeutic options and receive clear explanations of the risks (given that they may be fearful about the safety of certain treatments, especially in the case of systemic medications). Risks should be contextualized, for example: The risk of having side effects with this medication is lower than the risk of having an accident doing other daily activities. This medicine can cause X, and although this happens very rarely we will monitor you just in case. We have been using this medicine for many years to treat people with your disease. It is important to ensure that patients can correctly visualize the risk-benefit ratio: There is indeed a risk that you might develop pneumonia, but this medication also offers you a chance that all the lesions and itching you are experiencing will disappear; think about what that would mean to you.
Recommendation 10When the patient experiences a flare following a period during which the condition was controlled, the physician should explain that this is the normal course of the disease and work to build confidence in the dermatological treatments and reinforce the therapeutic relationship with the patient (LE, 5; GR, D; LA, 100%).
Although the treatments currently available are very effective, some patients will experience recurrent flares of the disease.60 Many of them will feel frustrated and anxious and they will relive the negative experience they had at the beginning when the disease was first diagnosed.
In the first place, the panel considers it important to emphasize that the patient should be made aware of this possibility; it should not take them by surprise. One way to do this, as described above, is to be forthright from the outset and to talk openly, without dramatizing, about the possibility of relapses. To reinforce the message that we are here, that we are going to closely monitor you and we will help you if a flare-up occurs: You can continue to rely on treatments. The response was very good once, there is no reason for it to be different in the future. There are many therapeutic options. Do not worry; you have been through this once, and I am here to make sure we resolve this outbreak too. These messages will strengthen the link between the patient and the dermatologist, making it clear that the management of the condition is ongoing and something they are undertaking together.
As this can be a difficult time for the patient, empathy is, once again, very important: I understand your worry and frustration.
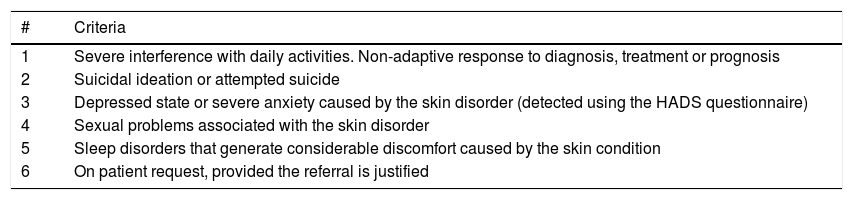
And finally, in Table 5 we summarize the criteria for patient referral to a mental health professional.
Criteria for Referring Patients With Chronic Inflammatory Skin Diseases to a Mental Health Specialist.
| # | Criteria |
|---|---|
| 1 | Severe interference with daily activities. Non-adaptive response to diagnosis, treatment or prognosis |
| 2 | Suicidal ideation or attempted suicide |
| 3 | Depressed state or severe anxiety caused by the skin disorder (detected using the HADS questionnaire) |
| 4 | Sexual problems associated with the skin disorder |
| 5 | Sleep disorders that generate considerable discomfort caused by the skin condition |
| 6 | On patient request, provided the referral is justified |
Abbreviation: HADS, Hospital Anxiety and Depression Scale.
Routine and specific screening for psychological symptoms in patients with chronic inflammatory skin diseases is justified because of the significant impact of such problems in these patients.3,10–12 To manage these conditions using a comprehensive approach, we need to be aware of and understand the psychological perspectives and needs of these patients.39
In this consensus document, we describe these psychological needs and propose a series of recommendations with practical examples for use in routine practice and adapted to the characteristics of the dermatology office. Moreover, since the patient's needs and our approach change over time and also because these depend on the characteristics of each patient, we have structured the recommendations around the initial stage of the disease and then the follow-up period, contemplating different scenarios that can have a specific psychological impact.60
One of the most innovative contributions of this document is the presentation of practical examples. These examples are intended to serve not just as a conceptual aid to cover a specific psychological need, but also to help physicians to achieve the greatest possible positive impact through effective communication.29–32 We also propose the use of the HADS questionnaire, a simple method for assessing patients with symptoms of anxiety and depression.42 We highlight the fact that in psoriasis, for example, the estimated prevalence of depressive symptoms or actual clinical depression can be as high as 30%.5–8 The information obtained using the HADS questionnaire can help us to determine whether referral to a mental health professional should be considered. For this purpose, we also propose a set of criteria for assessing whether such a referral is appropriate.
We should also point out that all of these recommendations achieved a high level of agreement during the Delphi process. This gives them greater value, especially in view of the fact that the panel included both dermatologists and psychologists and the paucity of the evidence available on this topic in the literature. Perhaps the recommendation that was most controversial (even though it reached the required level of agreement) was number 4, relating to the need to inform patients about patient associations, the resources they provide, and how they work. This may be due to the fact that in medical practice the explanations given to patients tend to focus closely on the disease process and the care and treatments for which scientific evidence is available or about which we have sufficient experience to support their recommendation. Although many medical professionals are clearly unaware of how patient associations work and their positive impact in this setting, published reports have shown that they can be very useful to patients with chronic inflammatory skin diseases.38
We also wish to highlight that the consensus statement includes a specific recommendation on sexual function, an area very much affected in these patients which is often not addressed due to taboos or a reluctance to talk about the subject.54,55
One of the limitations of this consensus document, as mentioned above, is the lack of scientific evidence to support many of the recommendations because of the lack of studies on the subject in the literature.
In conclusion, where psychological health is concerned, it is important not to overlook the emotional impact this group of diseases has on patients and their families.3,4 Psychological variables also play a fundamental role in other behaviors, such as adherence to treatment and the follow-up visit schedule.29–31 This document presents a set of recommendations relating to the psychological needs of patients with chronic inflammatory skin diseases, which we believe will serve as a practical guide to strategies clinicians can use in routine practice to help their patients. The panel was of the opinion that the application of these recommendations will improve communication with these patients and that they will serve as a useful reference for improving management of the psychological symptoms associated with these disorders.
FundingThis study was funded by Pfizer. Estíbaliz Loza of the Instituto de Salud Musculoesquelética (INMUSC), which is funded by Pfizer, provided assistance on methodological aspects and drafting the final document.
Conflicts of InterestSG and FR work for Pfizer. Pfizer did not have any input or influence on EL in the development of this consensus document. MR, RRV, SR, BM, and GC received honoraria from Pfizer for their collaboration and advice in the development of this document. All of the authors had access to the data and have contributed to the conceptualization and writing of the document. All of the authors declare that they have made a substantial contribution to this work and have reviewed the final manuscript. MR guarantees the overall content of this manuscript.
We thank Francisco Navarro Triviño; Manuel Galán Gutiérrez, Lourdes Rodriguez Fernandez Freire, Leandro Martinez Pilar, Alicia Gonzalez Quesada, Lucia Tomas, Esther Serra, Isabel Belinchón Romero, Marta García-Bustinduy, Servando Marrón Moya, Manel Velasco, Anna López Ferrer for their participation in the Delphi process.
Please cite this article as: Ribera M, Ros S, Madrid B, Ruiz-Villaverde R, Rebollo F, Gómez S, et al. Documento de consenso sobre las necesidades psicológicas de los pacientes con enfermedades inflamatorias crónicas dermatológicas. Actas Dermosifiliogr. 2019;110:102–114.