A 29-year-old black man, originally from Senegal, was referred for a suspected plantar melanoma. The patient reported a lesion that had developed 7 years earlier and made walking painful. Multiple treatments with antimicrobial agents in Senegal had led to no improvement. He reported no history of trauma, insect bite, or foreign body penetration and there was no significant medical history.
Physical ExaminationA lesion, measuring 6cm in diameter and covered by a hemorrhagic crust, was present on the sole of the patient's right foot. Removal of the crust revealed a suppurating surface with multiple fistulous tracts that produced a white-yellowish granular material (Fig. 1). Systemic examination showed signs of malnutrition (extreme thinness and diffuse alopecia).
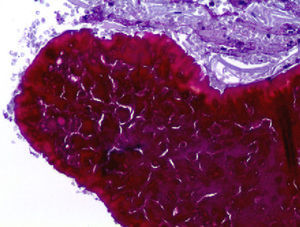
HistopathologyHistopathologic examination revealed orthokeratotic hyperkeratosis with underlying epidermal hyperplasia. The dermis showed a mixed, predominantly lymphoplasmacytic inflammatory infiltrate, vascular proliferation, and signs of chronic bleeding (Fig. 2). Clusters of gram-positive bacteria, forming structures with a basophilic granular center and peripheral eosinophilic collarette (Splendore–Hoeppli phenomenon), were observed using standard histochemical staining techniques (Fig. 3).
Additional TestsCulture of the exudate revealed Staphylococcus aureus and Streptococcus equisimilis. Radiographs of the chest, foot, and ankle were normal. Serology showed evidence of past infection with hepatitis B virus but was negative for human immunodeficiency virus. Other laboratory tests, including complete blood count, coagulation studies, biochemistry, liver and kidney function tests, and serology, were normal or negative.
What Is Your Diagnosis?
DiagnosisPrimary cutaneous botryomycosis.
Clinical CourseTreatment was started with oral amoxicillin (1g/8h) and clindamycin (300mg/8h) for 4 weeks, resulting in a significant reduction in the size of the lesion. Given the considerable clinical improvement with antibiotic treatment alone and in order to avoid surgery, the patient received oral cefadroxil (500mg/12h) for a further 4 weeks, with complete remission of the lesion.
DiscussionBotryomycosis is a chronic, granulomatous, suppurative bacterial infection that affects the skin and viscera. It is also known as staphylococcic actinophytosis, granular bacteriosis, and bacterial pseudomycosis.1 In 1884, Rivolta proposed the term botryomycosis to reflect the presumed fungal origin of the infection, and in 1914 Magrou identified S aureus as one of the causes of this disease.1-3
Botryomycosis represents a diagnostic challenge for many clinicians because fewer than 100 cases are described in the literature2 and it appears at different anatomical sites. The differential diagnosis should essentially include other granulomatous diseases such as actinomycosis, mycetoma, sporotrichosis, tuberculosis, leishmaniasis, and cutaneous carcinomas.4-8
The clinical course of botryomycosis, similar to that of chronic pyoderma, takes the form of a single lesion, which commonly affects exposed areas.1-3 The skin is the most frequently affected organ.2-4 The main causative agent is S aureus, followed by Pseudomonas aeruginosa, but the infection is polymicrobial in up to 50% of cases.7,8
The pathogenesis of the disease remains a subject of debate. It has been suggested that a balance between the number of microorganisms and the host's defences is necessary, as high concentrations of bacterial inoculum would cause extensive and rapid tissue necrosis, whereas low concentrations would cause the organisms to be phagocytized.1-8
Definitive diagnosis is based on histologic and microbiological criteria1-8 and is considerably aided by the study of the shape and characteristics of the granule for differentiation from actinomycosis and mycetoma (where granules are filamentous and change color rapidly with fungal stains). These studies also show the Splendore-Hoeppli phenomenon, when present. This phenomenon is highly characteristic of the disease and consists of periodic acid-Schiff–positive basophilic granules (clusters of bacteria), surrounded by eosinophilic material (immunoglobulin deposits), a reflection of the host's immune response.6
Administration of specific antibiotics for long periods forms the basis of treatment.2 Surgery is recommended when faster healing is required or there is only partial response to antibiotic treatment.1-6
Most cases in the literature describe patients with an abnormal immune function or significant comorbidities,3 but this was not true for our patient. Our patient had regularly walked barefoot in Senegal, a fact that, coupled with chronic malnutrition and irregular antibiotic treatment, could have contributed to the development and perpetuation of the disease.
Please cite this article as: Molina-Ruiz A, Pérez-Vega E, Zulueta-Dorado T. Úlcera plantar crónica en inmigrante africano. Actas Dermosifiliogr.2012;103:733-734.