Acquired generalized lipodystrophy (ALG) is a rare disorder characterized by the loss of adipose tissue and often found in association with metabolic disorders. Its onset is extremely rare in patients over 65 years, with only 1 case reported to date. Furthermore, there have been no reports of associated muscle involvement in ALG. We present the case of a 78-year-old woman who experienced almost complete loss of subcutaneous adipose tissue over 6 years. During this period, she was also successively diagnosed with hypertension, hypertriglyceridemia, hypothyroidism, hepatic steatosis, and diabetes mellitus. Possible causes of cachexia, such as infections, neoplasms, and gastrointestinal disorders, were ruled out. The patient's creatinine kinase levels were repeatedly elevated and electromyography showed a myopathic pattern, although the biopsy and strength tests were normal.
La lipodistrofia adquirida generalizada (LAG) es un trastorno raro caracterizado por un patrón característico de pérdida de tejido adiposo y frecuentemente asociado con trastornos metabólicos. El inicio tardío en mayores de 65 años es excepcional y se ha reportado solo en un único paciente.
Además, no se han publicado casos de LAG asociada a afectación muscular. Presentamos a una mujer de 78 años con pérdida prácticamente completa de su tejido adiposo subcutáneo a lo largo de los últimos 6 años. Además durante ese período fue sucesivamente diagnosticada de hipertensión, hipertrigliceridemia, hipotiroidismo, esteatosis hepática y diabetes mellitus. Enfermedades que pueden causar caquexia como infecciones, neoplasias o alteraciones gastrointestinales fueron descartadas. Sus niveles de creatinin kinasa fueron repetidamente elevados y su electromiograma mostró un patrón miopático aunque tanto la biopsia como las pruebas de fuerza fueron normales.
The lipodystrophies are a broad group of diseases defined by a variable degree of adipose tissue loss.1,2 They are classified into congenital or familial and acquired and subdivided into generalized, partial, and localized. The majority are associated with metabolic disorders that cause significant morbidity and mortality. Acquired generalized lipodystrophy (AGL) is a rare disorder that usually begins in childhood or youth; onset is rare in persons over 30 years of age. It is frequently associated with diabetes mellitus (89%), hepatomegaly (100%), hypertriglyceridemia (87.5%), and hyperinsulinemia (43%).3
We present the case of a patient with late-onset AGL associated with subclinical muscle involvement.
Case DescriptionThe patient was a 78-year-old woman with a 5-year history of hypertension, hypertriglyceridemia, hypothyroidism, and fatty liver. At the time of presentation she was on treatment with fenofibrate, levothyroxine, lisinopril, lorazepam, and calcium supplements. She reported weight loss of 15kg that had started 6 years earlier, prior to the onset of her other diseases, and also described the progressive appearance of prominent vessels on her trunk and limbs. She denied any changes in eating habits and did not report general or infectious symptoms (including gastrointestinal symptoms, myalgia, or weakness) or having taken drugs possibly related to weight loss. On physical examination there was an almost complete absence of fat, with prominence of the superficial veins and muscle pseudohypertrophy, as well as a characteristic facial appearance with loss of the Bichat fat pads (Fig. 1). There was hepatomegaly of 6cm, but no splenomegaly or pathologic lymph-node enlargement. There were no identifiable skin lesions, such as acanthosis nigricans or xanthomas. A deep skin biopsy that included muscle tissue revealed a normal epidermis and dermis, normal muscle tissue with no inflammatory infiltrate, and an absence of adipocytes.
A, Progressive loss of facial fat that can first be appreciated in the photographs from 2006 and that is particularly noticeable in the year prior to diagnosis. B, C, and D, Anterior, posterior, and lateral whole-body photographs showing almost complete loss of the subcutaneous cellular tissue. The lateral photograph (D) shows marked abdominal prominence.
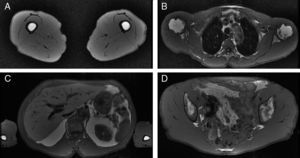
Blood tests showed a normal fasting blood glucose, elevated very low-density lipoproteins (around 65mg/dL), triglycerides of 250 to 300mg/dL, and decreased high-density lipoprotein (HDL) levels (around 32mg/dL) despite her lipid-lowering treatment. Creatine kinase values were increased to 250 to 350IU/L in serial blood tests (normal range, 1-167 IU/L), and lactate dehydrogenase and the transaminases were within normal limits. Autoimmunity studies were positive for antinuclear antibodies (titer, 1/160) and for anti-Ro/SSA. Other antibodies (SSB, Smith, ribonucleoprotein, Jo1, antineutrophil cytoplasmic antibody, and antiglomerular basement membrane) were negative. Diabetes mellitus with hyperinsulinemia was diagnosed on the basis of an abnormal oral glucose tolerance test associated with elevated levels of insulin and C-peptide. Complement (C3 and C4), protein electrophoresis, immunoglobulins, and the other hormones studied (testosterone, follicle stimulating hormone, luteinizing hormone, prolactin, dehydroepiandrosterone sulfate, androstenedione, intact parathyroid hormone, growth hormone, cortisol) presented values within normal limits. Serology for human immunodeficiency virus and hepatitis B and C viruses was repeatedly negative. Gastrointestinal absorption studies revealed no abnormalities, as no fats, proteins, or sugars and no parasites were found in the feces; the albumin, vitamin B12, folic acid, ferritin, and transferrin levels were within normal limits. Antigliadin and antitransglutaminase antibodies were not detected. The presence of underlying neoplastic disease was excluded on the basis of various imaging studies (high-resolution thoracic computed tomography, abdominal ultrasound, and parathyroid nuclear scan) and repeatedly negative tumor markers. The body fat percentage (measured by impedancemetry) was 16.4% (normal range, 25%-30%). An ultrasound study showed symmetrical loss of the adipose tissue, which had a maximum thickness of 2.9mm. T1-weighted magnetic resonance imaging demonstrated an almost complete absence of subcutaneous fat, with preservation of intra-abdominal and bone-marrow fat (Fig. 2). An electromyogram revealed a myopathic pattern, with shorter and low-amplitude motor-unit potentials associated with some fibrillation potentials. The patient was diagnosed with AGL on the basis of the combined data from the history, physical examination, and additional tests. Since diagnosis, the patient has been treated jointly in the dermatology and nutrition departments, with the administration of various antidiabetic drugs, including the thiazolidinediones, and lipid-lowering drugs with the aim of achieving good control of her multiple metabolic disorders.
T1-weighted magnetic resonance images.
A, Thighs, showing preservation of the intramedullary fat with an absence of subcutaneous and interfascicular fat. B, Thorax, with reduced intrathoracic fat and loss of subcutaneous adipose tissue. C, Abdomen with intraperitoneal fat, hepatomegaly, and an absence of subcutaneous fat. D, Pelvis: gluteal muscles of normal size.
AGL, also known as Lawrence syndrome, is a sporadic disorder described by Ziegler in 19284 and characterized clinically by Lawrence in 1964.5 It is divided into 3 groups: 1) post-panniculitis, which accounts for 25% of cases, in which the lipodystrophy is preceded by erythema nodosum; 2) autoimmune, which accounts for a further 25% of cases and can be associated with dermatomyositis, Hashimoto thyroiditis, and other autoimmune diseases; and 3) idiopathic, which accounts for 50% of reported cases and, as in our case, has no clear trigger.
Onset in patients over 65 years of age is very rare. Iglesias et al.6 reported the only case with similar characteristics to our patient in a woman of 74 years of age with poorly controlled diabetes mellitus and an increased excretion of fat in the feces. In our patient we excluded poor control of her endocrine diseases and other conditions that could lead to cachectic states, such as steatorrhea. Furthermore, our case satisfies all the diagnostic criteria for AGL proposed by Garg and Misra3 (Table 1), in the absence of triggering factors, and onset at an advanced age was confirmed by the medical history and previous photographs of the patient. This is therefore a true case of late-onset AGL, a condition rarely reported in dermatology journals.
Diagnostic Criteria for AGLa.
| Essential | Loss of fat affecting large areas of the body with onset after birth (usually in prepuberty) |
| Supporting | |
| Clinical | Loss of palmar-plantar fatAcanthosis nigricansHepatosplenomegalyPanniculitis in past history or on biopsyPresence of autoimmune diseases |
| Additional tests | Glucose intolerancePostprandial hyperinsulinemiaHypertriglyceridemia or low levels of high-density lipoproteinsLow levels of leptin or adiponectinLoss of subcutaneous fat evidenced on magnetic resonance imaging or anthropometryPreservation of bone marrow fat evidenced by magnetic resonance imaging |
Muscle alterations, on the other hand, have only been reported in lipodystrophies associated with dermatomyositis and in certain lipodystrophic syndromes associated with mutations in laminin (Dunnigan-type familial partial lipodystrophy7 and partial acquired lipodystrophy8). These types of lipodystrophy typically present clinical, histopathologic, enzymatic, and electromyographic alterations of the muscle. In our case, after 3 years of follow-up with only electromyographic and enzyme alterations, we believe it unlikely that a true myositis will develop. In our review of the literature we found no other cases of AGL with muscle disorders. We cannot rule out that the coexistence of both disorders in our patient (late-onset lipodystrophy and muscle disease) may be related to some currently unknown factor.
A promising drug for the treatment of AGL is recombinant human leptin,9 which is injected subcutaneously. However, its limited availability outside of clinical trials and the fact that it does not improve the physical appearance of patients10 means it is not usually prescribed. Lifestyle modifications and other more conventional therapeutic strategies, such as insulin, metformin, and thiazolidinediones to control the blood glucose, as were undertaken in our patient, are the most frequently recommended therapeutic options at the present time.
Finally, we would like to stress the importance of the ability of the dermatologist is to recognize this disease in order to perform correct screening and look for associated alterations, mainly of a metabolic nature, such as hepatomegaly secondary to fatty liver, glucose intolerance, hyperinsulinemia, and alterations of the lipid profile with reduced HDL and increased triglyceride levels, as these are the factors that determine the patient's prognosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr Abhimanyu Garg for his advice and for his help in establishing the diagnosis and Dr Ocón for her assistance in the interpretation of the imaging studies.
Please cite this article as: Llamas-Velasco M, Daudén E, Martínez-Peñas G, García-Diez A. Lipodistrofia generalizada adquirida de inicio tardío y con afectación muscular. Actas Dermosifiliogr.2012;103:729-732.