Dermal melanocytoses are a broad group of congenital or acquired melanocytic lesions that share the histopathologic feature of dendritic melanocytes in the dermis, with variable degrees of pigmentation and with or without dermal melanophages.1 This group includes the mongolian spot, blue nevus, nevus of Ota, nevus of Ito, Hori nevus and other less frequent entities, known as atypical dermal melanocytoses.2
We present the case of a 35-year-old Nigerian woman who consulted for progressive asymptomatic facial hyperpigmentation that had started to develop on her forehead 2 years earlier. The only finding in her past medical history was systemic hypertension, for which she was on treatment with amlodipine. She described no temporal relationship between taking amlodipine or other drugs and onset of the hyperpigmentation, and she denied taking other drugs or applying topical products to the area. No treatment had been performed.
The patient, with skin phototype V, presented multiple confluent macules of a few millimeters in diameter on her forehead, also extending into both parietal regions, grouped so as to form a large, poorly defined, bluish-gray macule of mottled appearance. The macule was not infiltrated and no superficial desquamation was observed (Fig. 1). No lesions were observed in the conjunctiva or on the oral mucosa.
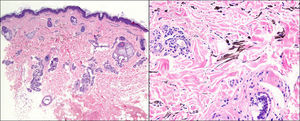
Biopsy revealed a proliferation of dendritic melanocytes in the mid dermis, with no atypia (Fig. 2), confirmed with Masson-Fontana stain. No nonmelanic pigment deposits were observed. All the findings were compatible with Hori nevus.
Hori nevus, also known as ABNOM (acquired bilateral nevus of Ota-like macules), is one of the most common acquired facial dermal melanocytoses.1 It was first described by Hori et al.3 in 1984. It usually affects Asian women in the fourth or fifth decade of life. Familial cases have been reported.4 Hori nevus presents as blue-gray-brown macules with a bilateral distribution on the forehead, frontoparietal regions, eyelids, cheeks, and nose. There is no associated ocular or mucosal involvement,3 although a case with mucosal involvement has recently been described. We consider that the clinical and pathologic findings of that case with mucosal involvement could correspond to a nevus of Ota.5
The origin of this alteration is unknown. The etiology and pathogenesis of Hori nevus appear to require the presence of poorly melanized ectopic melanocytes in the dermis, by descent or migration from the epidermis or hair bulb (dropping off) or by disturbances of migration during embryologic development, and the activation of these cells by UV radiation, hormones, chronic inflammation, or other as yet undefined factors.1 Diagnosis is mainly clinical. Histopathology reveals melanocytes in the mid and upper dermis, with no fibrosis or alterations of normal dermal structure.3 Ultrastructurally, these melanocytes are fully developed, with stage II, III and IV melanosomes, and are surrounded by an extracellular sheath whose thickness increases over time, leading to lesion stability.1,3
The main differential diagnoses are nevus of Ota, Riehl melanosis, ochronosis, and melasma.3 Nevus of Ota is differentiated by an earlier age at onset, a unilateral presentation, and mucosal involvement. Riehl melanosis and exogenous ochronosis are associated with a history of application of topical products prior to appearance of the lesions. In endogenous ochronosis, nonmelanic pigment is observed in the dermis. Melasma shares certain clinical characteristics, such as a female predominance, involvement typically of the malar region, and a common pathogenesis with increased expression of the SCF/c-kit pathway,6 but the bluish-gray color of Hori nevus is not observed,3,7 and histopathologic findings are also different.8,9 Histopathologic studies with healthy controls, the reported findings characteristic of melasma are increased melanin deposits in the epidermis, with normal or increased presence of epidermal melanocytes, which can appear larger than usual, with prominent dendrites, sometimes associated with an increase in the number of melanophages.8,9 Based on these findings, although melasma has been subclassified into epidermal and dermal, it is likely that the purely dermal forms are actually Hori nevus.8
With regard to treatment, some authors report improvement with various Q-switched (QS) lasers (QS yttrium-aluminium-garnet laser [1064nm], QS alexandrite laser [755nm], and QS ruby laser [694nm]), though results are variable and a transitory residual hyperpigmentation is the norm.1,10–13 To reduce this residual hyperpigmentation combined treatments with QS laser and bleaching agents, dermabrasion, or carbon dioxide laser have been used.1,12
In conclusion, Hori nevus is a cause of acquired facial hyperpigmentation that should be considered in daily clinical practice.
Please cite this article as: González-Olivares M. Hiperpigmentación facial simétrica adquirida. Actas Dermosifiliogr. 2016;107:355–357.